13 Focused Assessment: Nutritional Assessment
Learning Objectives
At the end of the chapter, the learner will:
- Relate concepts of nutrition and metabolism with GI assessment and elimination.
- Identify patients at risk for developing malnutrition.
- Use nutritional assessment in the provision of health care.
- Document findings using correct medical terminology.
I. Overview of Nutritional Assessment
Proper nutrition is important to maintain health and prevent illness. Health care providers must routinely evaluate patients’ nutritional status and to identify any existing or potential nutritional problems. This allows for appropriate referrals and interventions to be provided.
Various physical conditions can disrupt nutritional absorptions. For example, patients with gastrointestinal problems such as inflammatory bowel disease or liver cirrhosis may experience malnutrition. Those with lung problems might have insufficient oral intake due to breathing difficulties. Diabetes patients often face inadequate glucose homeostasis. Psychiatric disorders or depression can lead to functional impairments that cause poor nutritional intake. Cancer patients may suffer from cancer cachexia and malnutrition, and those in pain might decrease their oral intake.
Many medications can also interfere with nutritional absorptions. Diuretics, for example, may cause dehydration and electrolyte imbalances. Narcotics and opioids can lead to nausea and vomiting, while anticholinergic drugs may cause dry mouth, affecting food intake.
Malnutrition is defined as “deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients” (WHO, 2021). According to the World Health Organization (WHO), malnutrition encompasses several conditions:
- Undernutrition: Wasting (low weight-for-height), stunting (low height-for-age), and underweight (low weight-for-age).
- Micronutrient-related malnutrition: Deficiencies or excesses in vitamins or minerals.
- Overweight, obesity, and diet-related noncommunicable diseases (NCDs): A body mass index (BMI) over 25 kg/m2 is considered overweight, and a BMI above 30 kg/m2 is classified as obesity. Diet-related NCDs include cardiovascular disease, diabetes, and certain cancers (such as liver cancer or oral cancer).
Body Mass Index (BMI) estimates body fat using a person’s weight and height. Research has shown that BMI is highly correlated with many metabolic and cardiovascular diseases (CDC, nd.) and is recommended as the primary screening method for weight control and metabolic health assessment. However, BMI has limitations, as it cannot distinguish between fat and lean body mass or subcutaneous fat. Measuring waist circumference to assess abdominal fat is critical and is strongly associated with NCDs (Yurista et al., 2023).
BMI Calculator
Click the link of BMI Calculator and follow the instructions to calculate your BMI (NHLBI, nd.).
| BMI (kg/m2) | Status |
| Below 18.5 | Underweight |
| 18.5 – 24.9 | Normal weight |
| 25 – 29.9 | Overweight |
| Above 30 | Obese |
II. Anatomy and Physiology
Digestion begins in the mouth, where chewing and mixing with saliva initiate the breakdown of food. In the stomach, food mixes with gastric juices to produce a mixture called chyme. Chyme then passes into the small intestine, where most digestion takes place. In the small intestine, food is dissolved, and nutrients are absorbed into the body. Unabsorbed wastes are passed down to the colon.
Nutrients are divided into macronutrients and micronutrients. Macronutrients refer to carbohydrates, fats, and proteins that must be consumed daily to produce energy and ensure proper bodily function.
Watch the following short video clip to review digestion in the small intestine.
Micronutrients refer to dietary minerals and vitamins that support the body’s metabolism.
The following short video clip provides information on the essential nutrients for life: minerals and vitamins.
Knowledge Check
III. Medical Terminology
| Anthropometry | measurement of the body ratios and sizes including height, weight, skinfold thickness, waist circumference, mid-arm circumference, and calf circumference |
| Body mass index (BMI) | a measure of body fat based on height and weight; a person’s weight in kilograms divided by the square of height in meters |
| Malnutrition | deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients |
| Obesity | is defined as abnormal or excessive fat accumulation that poses a risk to health; BMI >30 kg/m2 |
| Recommended dietary allowance (RDA) | the levels of intake of essential nutrients sufficient to meet the nutrient requirements of practically all healthy people |
| Failure to thrive | in the elderly, weight loss of more than 5%, decreased appetite, poor nutrition, and physical inactivity, often associated with dehydration, depression, and immune dysfunction; a state of decline |
IV. Nutritional Assessment
Nutritional assessment is an ongoing component of daily assessment, especially for patients with nutritional concerns and those at risk for nutritional deficits.
| Screening for Nutritional Status | Additional Information |
1. Obtain health history
|
Dietary and nutritional differences can be found among racial and socioeconomic groups.
Dietary selections can be affected by religious, spiritual, or philosophical beliefs. |
2. Obtain chief complaints
|
Chief complaints should be considered because it may indicate the patient to be at risk for nutritional deficits.
Problems with intake such as indigestion, heartburn, bloating, difficulty chewing or swallowing will affect nutritional status. If the patient has a specific concerns about hair, skin, or nails, a focused assessment regarding to the specific sign/symptom should be performed.
|
3. Check
|
Note the size of the patient and calculate BMI to determine normal, overweight, or obesity.
Waist circumference can also be measured for adult patients to determine if they are at risk for cardiovascular disease. A normal waist circumference should be less than 40 inches for men and less than 35 inches for women. However, there are variations in waist circumference and cardiovascular risk among different ethnic backgrounds (Yurista et al., 2023). 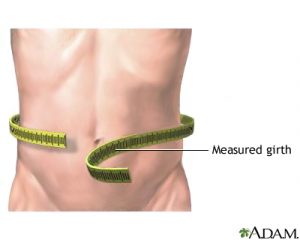 |
4. General inspection and examination
|
During mealtime, observe the patient’s dietary intake and compare it with the recommended food groups for their specific age group and activity level.
Expected findings include alertness and orientation, a normal proportion of body structure, normal skin tone, and skin color appropriate to ethnicity, with no signs of malnutrition. Many diseases are directly or indirectly caused by a lack of essential nutrients in the diet. Changes in the skin and mucous membranes can offer valuable clues to the presence of nutritional deficiencies. For example, gingivitis and bleeding gums may be cause by vitamin C deficiency. In the integumentary system, malnourished patients are likely to have brittle and dry hair, or experience hair loss. The skin may appear pale, dry, and rough, and wounds may take longer to heal. Physical difficulties, such as tremors, can affect dietary intake. Nurses should assess if equipment is needed to assist with eating and drinking. |
| 5. Review related laboratory results | Some laboratory values that may reflect the patient’s nutritional status include albumin, prealbumin, transferrin, electrolytes, and lipid levels. |
| 6. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety.
Recommend additional nutritional evaluations, such as referral to a dietitian, to determine the need for nutritional supplements. |
General Assessment for Nutritional Status (Hinkle, 2021)
| Body Parts | Normal Findings | Signs of Poor Nutrition (will require further assessment) |
| Appearance | alert and oriented | lack of energy |
| Weight | normal for height and age | overweight or underweight |
| Face | consistent skin color | face swollen, skin flaky |
| Lips | pink color, smooth | swollen and puffy, lesion at the corner |
| Tongue | papillae present | smooth and shiny appearance of the tongue with loss of papillae |
| Gums | pink color, firm | inflammation, swollen, and bleeding |
| Hair | healthy scalp, shiny hair | fragile, thin, and sparse hair |
| Skin | smooth, color appropriate to ethnicity | rough, flaky, swollen, pale or yellowish appearance |
| Nails | pink | spoon nails, brown-gray nails |
| Skeleton/extremities | erect normal posture, no tenderness | bowed legs, weakness, tenderness |
| Abdomen | flat | swollen |
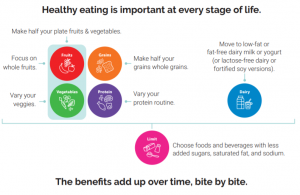
Access additional information to educate patients on healthy dietary patterns. The guidelines were developed by the U.S. Department of Agriculture (USDA) and the U.S. Department of Health and Human Services (HHS) to provide recommendations on healthy eating, promoting health, and preventing chronic illness. These guidelines include recommendations for all stages of life, from birth through older adulthood, as well as for women who are pregnant or breastfeeding.
Knowledge Check
V. Documentation of Assessment Findings
Sample Narrative Documentation
Patient was admitted with peptic ulcer this morning. Continues to experience decreased appetite and intermittent epigastric pain, rates 2 on 0-10 pain scale currently. Abdomen soft, distended, and tender to touch. Normal bowel sounds in all 4 quadrants. No bowel movement for 2 days. Pale skin color, warm, dry. Lips pale, oral mucosa moist and intact. Afebrile, BP 110/68, P 100, R 22. Denied shortness of breath. Clear lung sounds bilaterally. No acute distress. Declined pain medication. IV D5W in Left forearm at 50 mL/hr. NPO, wait for the scheduled upper endoscopy procedure.
VI. Related Laboratory and Diagnostic Procedures/ Findings
Nutritional assessment is an ongoing process for hospitalized patients. If assessment findings suggest nutritional concerns, such as inadequate oral intake or poor wound healing, further diagnostic and laboratory tests may be conducted to uncover underlining causes and provide nutritional support.
Certain laboratory results can help determine a patient’s nutritional status. Serum albumin and prealbumin levels are useful for assessing patient’s protein requirements. Electrolytes (such as serum calcium, magnesium, and phosphorous), blood urea nitrogen (BUN), and creatinine can be evaluated to assess fluid volume status and the need for parental nutrition. If diet-related noncommunicable or metabolic diseases are suspected, glucose and lipid levels (total cholesterol, LDL, HDL, and triglycerides) may be assessed. Transferrin, a protein that transports iron through the blood to various tissues and organs, can indicate protein status. Low transferrin levels may signal iron deficiency and anemia. In the evaluation of anemia, a complete blood count (CBC), serum iron level, serum vitamin B12, and folate levels are also checked. Additionally, blood tests for specific vitamin deficiencies may be necessary for patients with gastrointestinal malabsorption (Hinkle, 2021).
Click the link to access additional nutritional assessment OERs: Nutrition.
VII. Learning Exercises
Self Learning Activity
Target 3.4 – By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
Indicator 3.4.1 – Mortality rate attributed to cardiovascular disease, cancer, diabetes or chronic respiratory disease.
Activity Title: Nutritional Assessment: Unveiling the Path to a Healthier You!
Objectives of this Activity:
You will be able to
-
- Assess your current eating pattern and gain insight into your nutritional status and overall well-being.
- Identify any imbalances in your diet and take appropriate steps to address them.
Instructions:
- Write out a typical day of meals – breakfast, lunch, dinner, snacks.
- Click MyPlate Plan link: MyPlate Plan.
- Click on the “Start” button.
- Enter your age, sex, height, weight, and physical activity level.
- Click “Calculate food plan” to find your personal plate plan.
- Evaluate your food intake against the recommended plan in the food group amounts – fruits, vegetables, grains, protein, and dairy.
Self-Evaluation Questions:
- What changes do you need to make?
- Explain how you can integrate nutritional knowledge into your daily life and make informed decisions about your diet, ultimately leading to improved overall health outcomes.
VIII. Attribution and References
- Centers for Disease Control and Prevention. Healthy Weight, Nutrition, and Physical Activity: About adult BMI. Available at https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#InterpretedAdults
- Ernstmeyer, K., & Christman, E. (Eds.). (2021). Open RN Nursing Fundamentals by Chippewa Valley Technical College is licensed under CC BY 4.0.
- Hinkle, J. (2021). Brunner & Suddarth’s Textbook of Medical-surgical Nursing. (15th ed.). Philadelphia, PA: Wolters Kluwer.
- National Heart, Lung, and Blood Institute. Calculate Your Body Mass Index. Available at https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
- United Nations. Sustainable Development Goals. https://sdgs.un.org/goals
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov
- World Health Organization. Malnutrition. 9th June 2021. Available at https://www.who.int/news-room/fact-sheets/detail/malnutrition.
- Yurista, S. R., Eder, R. A., Feeley, M., Kodur, N., Tang, W. H., & Nguyen, C. T. (2023). A closer look at ACC/AHA and ESC guidelines for managing obesity and overweight in adults. Journal of American College of Cardiology Advances, 2(7). https://doi.org/10.1016/j.jacadv.2023.100570

