15 Focused Assessment – Integumentary System (Hair, Skin and Nails)
Learning Objectives
At the end of the chapter, the learner will:
- Obtain a health history of the integumentary system.
- Describe variations of normal findings of the integumentary system
- Describe common lesions of the skin, hair, and nails.
- Perform physical assessment of the integumentary system using correct techniques of assessment.
- Document the integumentary system assessment.
I. Overview of Assessment of the Integumentary System
The assessment of the integumentary system which includes the skin, hair and nails is an important element of the nurse’s assessment of the patient’s health status. These body structures do have specific functions but they also reflect functions or dysfunctions of other body systems as well. This chapter presents important concepts that will prepare the nurse to assess the patient’s integumentary system.
II. Review of Anatomy and Physiology
In the following video, structures and functions of the integumentary system are reviewed. Knowledge of anatomy and physiology of the body systems is essential to the assessment process as the nurse compare normal expected findings and patient manifestations.
More Reviews on Integumentary System
Additional information can be accessed through the following links:
III. Medical Terminology:
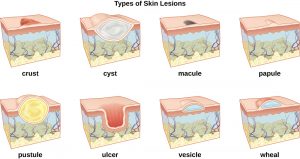
| Abscess | a localized collection of pus caused by infection. |
| Bullae | fluid-filled, elevation, superficial lesion greater than 1 cm in diameter |
| Crust | is resulted from the dried secretions over the skin |
| Cyanosis | bluish-gray discoloration of the skin resulting from the presence or abnormal amounts of reduced hemoglobin in the blood |
| Cyst | a closed sac containing liquid or semisolid material |
| Ecchymosis | discoloration of skin caused by leakage of blood into the subcutaneous tissue |
| Excoriation | scratch or abrasion on the skin surface |
| Fissure | linear crack in the skin surface |
| Macule | flat, circumscribed lesion of the skin or mucous membrane that is 1 cm or less in diameter |
| Nodule | solid skin elevation that extends into the dermal layer and that is 1 to 2 cm in diameter; a form of papule but larger and deeper |
| Papule | solid, elevated, superficial lesion 1 cm or less in diameter |
| Petechiae | tiny, flat purple or red spots on the surface of the skin resulting from little bleeding within the dermal or submucosal layers |
| Pruritus | itchy skin |
| Purpura | hemorrhage into the tissue, usually circumscribed; lesions may be described as petechiae, ecchymoses according to size |
| Pustule | vesicle or bullae that contains pus |
| Ulcer | Circumscribed open wound on the surface of the skin or mucous membrane |
| Urticaria | Hives; raised and itchy skin that is usually a sign of an allergic reaction |
| Vesicle | fluid-filled, elevation, superficial lesion 1 cm or less in diameter |
| Wheal | flat-topped elevation in the skin that is edematous and erythematous |
Knowledge Check

IV. Step by Step Assessment
Safety considerations:
- Perform hand hygiene.
- Check room for contact precautions.
- Introduce yourself to patient.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain process to patient.
- Be organized and systematic in your assessment.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure patient’s privacy and dignity.
- Apply principles of asepsis and safety.
- Check vital signs.
| Steps | Additional Information |
Please note: Assessing the skin, hair, and nails is an ongoing element of a full body assessment. In certain instances, a comprehensive or focused skin assessment must be performed, such as assessing risk factors for pressure ulcers.
|
|
| Skin, hair, and nails:
4. Inspection:
5. Palpation:
|
Check hair for the presence of lice and/or nits (eggs), which are oval in shape and adhere to the hair shaft.
Check for and follow up on the presence of lesions. Note any changes in color such as cyanosis, erythema, jaundice, or pallor. Variations in skin temperature, texture, and perspiration or dehydration may indicate underlying conditions. Redness of the skin at pressure areas such as heels, elbows, buttocks, and hips indicates the need to reassess patient’s need for position changes. Unilateral edema may indicate a local or peripheral cause, whereas bilateral-pitting edema usually indicates cardiac or kidney failure. Check skin turgor: use the thumb and index fingers to pinch an area of the skin and release it. It should instantly return to place. Use The Braden Scale to identify patients who are at risk for pressure injuries. |
| 6. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety. |
Note: Click all hyperlinks to access more details. Copyrighted materials used with permission of the author, A. Chandrasekhar, Loyola University Medical Education Network.
Braden Scale
The Braden scale is an evidence-based assessment tool frequently used in health care to identify patients who are at risk for pressure injuries, and then to provide early interventions to prevent or reduce the injuries. The tool includes assessment in 6 categories that may potentially cause pressure injuries: sensory perception, moisture, activity, mobility, nutrition, and shear/friction. It will generate a total risk score ranging from 6 to 23. The lower the score, patients will be more likely to increase the risk of developing pressure injuries. Click on the link to access detailed description of The Braden Scale.
Knowledge Check
More integumentary system health assessment open educational resources are available with a click: Nursing Skills – Integumentary Assessment.
V. Documentation
A sample narrative documentation:
Skin warm, dry/clean/intact, color appropriate for ethnicity. Well hydrated with normal skin turgor. Full hair distribution on scalp, and normal hair distribution on arms and legs. Nails neatly trimmed, 160-degree angle at base. Capillary refill < 3 sec. Denies skin itchiness. No lesions noted.
VI. Related Laboratory and Diagnostic Procedures/Findings
Some diagnostic tests may be done to assist in diagnosing integumentary concerns.
- A skin biopsy is a procedure that removes a small sample of skin tissue to diagnose skin cancer or other skin problems.
- Patch testing is performed to identify specific substances that cause allergic reaction in patients. Suspected allergens are applied on the skin of the patient. After 48 hours, if signs and symptoms of redness, elevations, itching, blisters, papules, and/or pain develop, it is considered a positive reaction to the allergen (Hinkle & Cheever, 2018).

- Wood’s light or Wood’s lamp examination is to use long wave ultraviolet light to detect skin infections or disorders (Al Aboud & Gossman, 2021).
VII. Learning Activities:
VIII. Citations and Attributions
- Al Aboud D.M., & Gossman, W. (Updated 2021 Jan 22). Woods Light. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537193/
- Andersen, P. (2014). Integumentary System. Bozeman Science. https://www.youtube.com/watch?v=z5VnOS9Ke3g
- Carter, K. & Rutherford, M. Building a Medical Terminology Foundation. https://ecampusontario.pressbooks.pub/medicalterminology/chapter/integumentary-system/
- Chandrasekhar, A. Screening physical exam. March 2006. http://www.meddean.luc.edu/lumen/MedEd/medicine/pulmonar/pd/pstep75.htm
- Doyle, G. R. & McCutcheon, J. A. Step by Step Checklist adapted from https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/
- Ernstmeyer, K., & Christman, E. (Eds.). (2021). Open RN Nursing Skills by Chippewa Valley Technical College is licensed under CC BY 4.0.
- Ernstmeyer, K., & Christman, E. (Eds.). (2021). Open RN Nursing Fundamentals by Chippewa Valley Technical College is licensed under CC BY 4.0.
-
Hinkle, J. L. & Cheever, K. H. (2018). Brunner & Suddarth’s Textbook of Medical-surgical Nursing. (14th ed.). Philadelphia, PA: Wolters Kluwer.
- Wikibooks. (April 2021 updated). Human Physiology/Integumentary System. https://en.wikibooks.org/wiki/Human_Physiology/Integumentary_System Accessed July 20, 2021
- Zulkowski, K. (2017). Comprehensive skin assessment. https://www.youtube.com/watch?v=L1OpaWDAv_A&t=4s

