14 Focused Assessment- Musculoskeletal System/Mobility
Ching-Chuen Feng
Learning Objectives
At the end of the chapter, the learner will:
- Obtain a health history related to the musculoskeletal system.
- Perform physical examination of the musculoskeletal system using correct examination techniques.
- Assess the ability to perform activities of daily living.
- Discuss screening tools for falls risk assessment.
- Document the findings from the musculoskeletal assessment.
I. Overview: Focused Musculoskeletal System Assessment
A focused musculoskeletal assessment includes collecting subjective data about the patient’s mobility and exercise level, as well as the patient’s and family’s history of musculoskeletal conditions. The nurse should ask the patient about any signs and symptoms of musculoskeletal injury or conditions. Objective data will include assessing the patient’s range of motion and muscle strength. Additionally, the patient should be evaluated for fall risk.
II. Anatomy and Physiology Review:
III. Medical Terminology
Important Terms to know:
| Ankylosis | fixation of a joint, usually resulting from destruction of articular cartilage |
| Ataxia | inability to coordinate muscular movement |
| Bradykinesia | abnormal slowness of movement |
| Crepitus | a grating, creaking, or cracking sound or sensation heard or felt when moving a join |
| Dyskinesia | uncontrolled, involuntary movements |
| Erythema | redness of the skin |
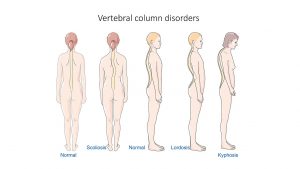
| Kyphosis | abnormal outward curvature of the spine |
| Lordosis | abnormal inward curvature of the lumbar spine |
| Muscle strength | the muscle’s ability to contract and create force in response to resistance |
| Muscle tone | the tension in a muscle at rest |
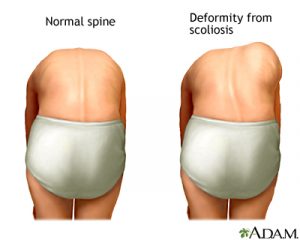
| Scoliosis | lateral curvature of the spine |
| Sprain | traumatic injury to the ligament |
| Strain | traumatic injury to the muscle or the tendon |
| Tendinitis |
inflammation of a tendon |
Illustrations of normal and abnormal spinal curvatures
The normal spine should be straight with expected curvatures, and the body should be symmetrical when comparing one side to the other.
Range of Motion (ROM) Terms:
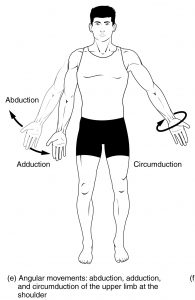
| Abduction | movement of a limb away from the body |
| Adduction | movement of a limb toward the body |
| Circumduction | circular movement of a limb |
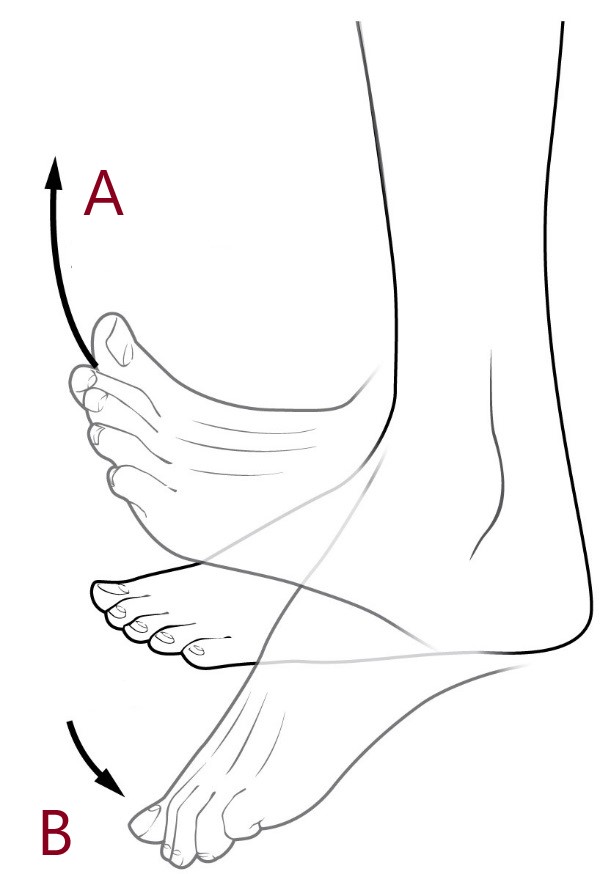
| Dorsiflexion | backward or upward motion of a body part |
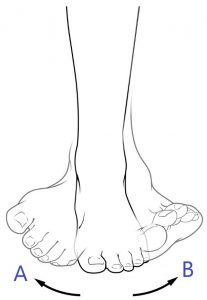
| Eversion | turning the sole of the foot away from the midline |
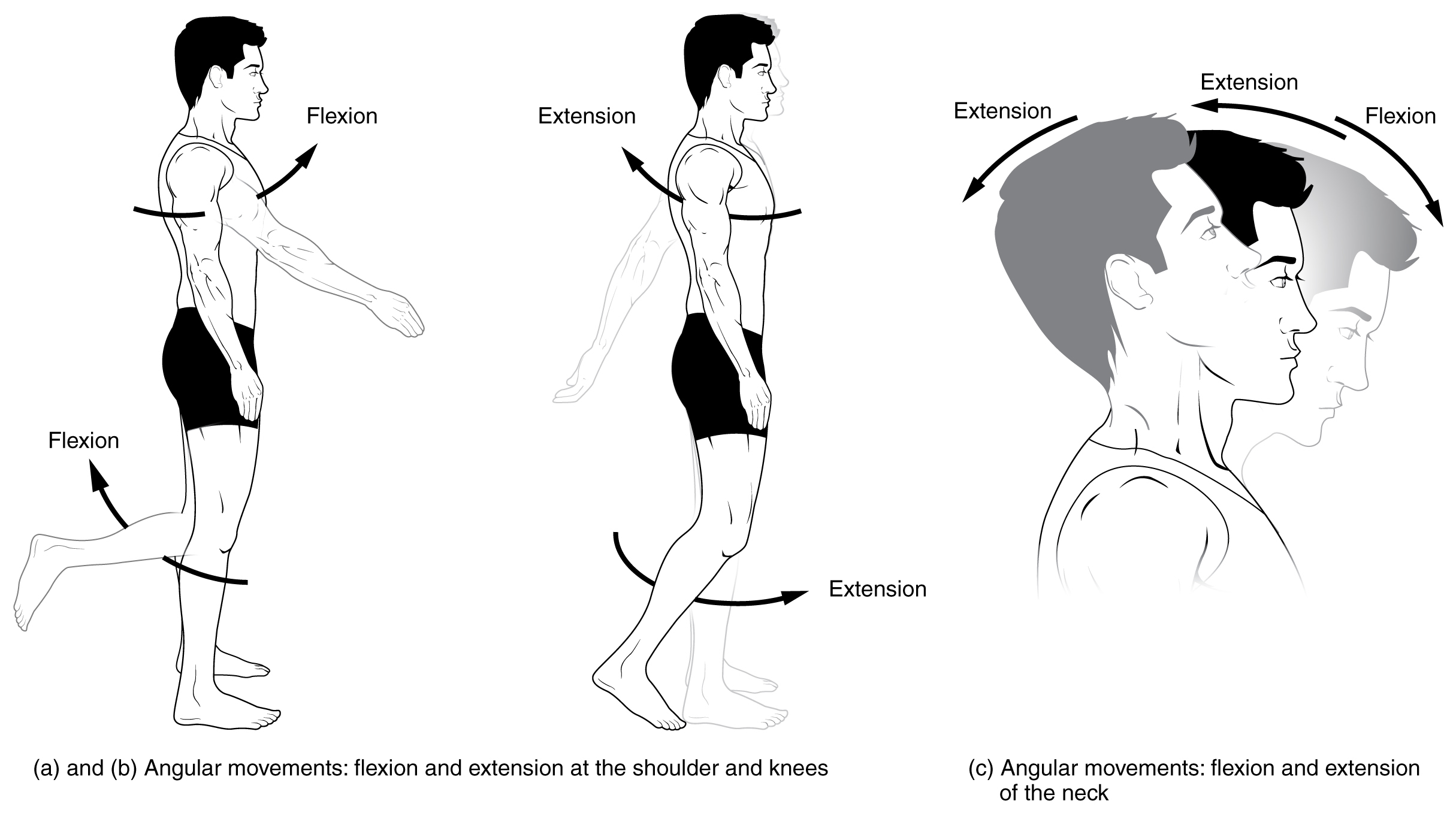
| Extension | movement of bringing a joint into a straight position |
| External Rotation | or lateral rotation, turning a limb outward from the mid line of the body |
| Flexion | movement that brings a joint into a bent position |
| Hyperextension | extension of a body part beyond normal limits of extension |
| Internal Rotation | inward turning of a limb |
| Inversion | turning the sole of the foot inwards towards the midline |
| Supination | turning the forearm to keep palm facing up |
| Plantar Flexion | bending of the foot or toes toward the sole of the foot |
| Pronation | turning the forearm to keep palm facing down |
| Rotation | turning the head to the left or the right |
Illustrations of Range of Motion:
Three types of ROM:
Active Range of Motion: Patient performs the exercise independently without any assistance.
Active Assisted Range of Motion: Patient moves the joints with some effort and requires some assistance from another person or equipment.
Passive Range of Motion: Patient does not perform any movement and depends totally on someone (therapist) or equipment to perform ROM.
Knowledge Check
IV. Step-by-step Assessment of the Musculoskeletal System
Safety considerations:
- Perform hand hygiene.
- Check room for contact precautions.
- Introduce yourself to patient.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain process to patient.
- Be organized and systematic in your assessment.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure patient’s privacy and dignity.
- Assess ABCCS/suction/oxygen/safety.
- Apply principles of asepsis and safety.
- Check vital signs.
| Steps |
Additional Information | ||||||||||||||
1. Check patient information prior to assessment:
2. Check alertness, medications, and pain levels. 3. Ask if the patient uses any assistive devices such as a walker, cane, wheelchair, or crutches. 4. Conduct a focused interview related to mobility and the musculoskeletal system. |
Determine patient’s activity as tolerated (AAT) or bed rest requirements.
Determine if patient has non-weight-bearing, partial weight-bearing, or full weight-bearing status. Determine if the patient ambulates independently, with one-person assist (PA), two-person assist (2PA), standby assist, or requires a lift transfer. Consider using non-slip socks, hip protectors, or a bed-chair alarm for safety. Ask relevant questions related to the musculoskeletal system, including pain, function, mobility, and activity level (e.g., arthritis, joint problems, medications, etc.). |
||||||||||||||
5. Inspect, palpate, and test muscle strength and range of motion:
|
If the patient states pain or tenderness in an area, conduct a further assessment.
The Adam’s Forward Bend Test is used to screen for scoliosis.
    |
||||||||||||||
| 6. Evaluate patient’s ability to sit up before standing.
7. Evaluate the patient’s ability to stand before walking. 8. Assess the patient’s walking ability.
|
 |
||||||||||||||
| 7. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety. |
Fall Risk Assessment
Falls are a significant problem for hospitalized patients. Several tools are available for assessing and identifying fall risk in these patients (Aranda-Gallardo et al., 2013). The Morse Fall Scale (Morse, Morse, & Tylko, 1989) is a widely used tool for identifying risk factors for falls and preventing potential falls in hospitalized patients.
The Morse Fall Scale includes six categories that reflect fall risk: history of falls, secondary diagnosis, ambulatory aids, intravenous therapy, gait, and mental status. The nurse tallies the scores from these categories to objectively evaluate the patient’s fall risk and then provides necessary interventions to prevent falls (AHRQ, n. d.).
Morse Fall Scale
| Item | Item Score |
Patient Score |
| 1. History of falling | 0- No
25- Yes |
|
| 2. Secondary diagnosis
(more than 2 medical diagnoses) |
0- No
25- Yes |
|
| 3. Ambulatory aids | 0- None/bedrest/nurse assist
15- Crutches/cane/walker 30 – Furniture |
|
| 4. Intravenous therapy | 0- No
25- Yes |
|
| 5. Gait | 0- Normal/bedrest/wheelchair
10- Weak (short steps) 20- Impaired (short steps with shuffle) |
|
| 6. Mental status | 0- Oriented to own ability
15- Overestimates/forgets limitations |
|
|
Total Score: |
Tally the patient’s score:
0: No risk for falls
<25: Low risk
25-45: Moderate risk
>45: High risk
Additional Information
Falls are also a significant concern for older populations living at home or in long-term care facilities. Access additional health information to educate patients on fall prevention strategies. Fall Risk Assessment: https://medlineplus.gov/lab-tests/fall-risk-assessment/
V. Documentation
A sample narrative documentation:
Patient denies problems with muscle weakness or tremor, no history of falls. Performs ADL independently, denies problems with mobility. Steady coordinated gait with erect posture, full ROM, muscle strength (5/5) equal and strong bilaterally in all joints with smooth and nonpainful movements, muscle size symmetric bilaterally, shoulders aligned, spine straight and in midline. No pain or tenderness on palpation.
VI. Related Laboratory and Diagnostic Tests
Some blood tests used to diagnose musculoskeletal problems include:
- Serum Calcium Levels: Abnormal levels can indicate osteomalacia or parathyroid problems.
- Rheumatoid Factor (RF): Used to diagnose rheumatoid arthritis, an autoimmune disease.
- HLA-B27: A specific gene tested for diagnosing ankylosing spondylitis, a disorder affecting the spine, pelvic bones, and hip joints.
- White Blood Cell Count (WBC), Erythrocyte Sedimentation rate (ESR), and C-Reactive Protein (CRP): These may be checked to diagnose infection or inflammation.
- Creatine Kinase (CK) or Creatine Phosphokinase (CPK): These enzymes are checked to diagnose muscular injuries such as myopathy, muscular dystrophy, or rhabdomyolysis. CK found in skeletal muscle, myocardium, and brain, will be elevated in the blood when muscle is damaged.
Some diagnostic tests used to diagnose musculoskeletal problems include:
- X-Ray Studies: Identify and evaluate bone density and structure.
- Computed Tomography (CT) Scan: Evaluates musculoskeletal trauma and bony abnormalities that may not able to be detectable with X-rays.
- Magnetic Resonance Imaging (MRI): Assesses problems in bones and soft tissues, including torn muscles, disk abnormalities, ligament or cartilage tears, and other hip or pelvic conditions.
- Bone Densitometry: Performed using X-rays or ultrasound to evaluate bone density in the spine, hip, wrist, and total body. It also predicts fracture risk and assesses treatment effectiveness for osteoporosis.
- Bone Scan: Examines the entire skeletal system to evaluate unexplained bone pain, detect damage from infection or other disease, and discover cancer in bones caused by metastasis.
- Arthroscopy: Uses a fiber-optic endoscope inserted into a joint to perform surgery and/or diagnose diseases of the patella, meniscus, and synovial membranes.
- Electromyography (EMG): Evaluates the electrical activity of muscles and nerves to diagnose neuromuscular diseases and motor or nerve problems (Hinkle & Cheever, 2018).
VII. Learning Activity
VIII. Citations and Attributions
- Agency for Healthcare Research and Quality (AHRQ). Tool 3H: Morse Fall Scale for Identifying Fall Risk Factors. https://www.ahrq.gov/patient-safety/settings/hospital/fall-prevention/toolkit/morse-fall-scale.html. Accessed July 15, 2021
- Aranda-Gallardo, M., Morales-Asencio, J. M., Canca-Sanchez, J. C., Barrero-Sojo, S., Perez-Jimenez, C., Morales-Fernandez, A., de Luna-Rodriguez, M. E., Moya-Suarez, A. B., & Mora-Banderas, A. M. (2013). Instruments for assessing the risk of falls in acute hospitalized patients: a systematic review and meta-analysis. BMC health services research, 13, 122. https://doi.org/10.1186/1472-6963-13-122
- Doyle, G. R. & McCutchen, J. A. Clinical procedures for safer patient care. https://opentextbc.ca/clinicalskills/chapter/introduction/
-
Hinkle, J. L. & Cheever, K. H. (2018). Brunner & Suddarth’s Textbook of Medical-surgical Nursing. (14th ed.). Philadelphia, PA: Wolters Kluwer.
- MedlinePlus. Forward bend test. https://medlineplus.gov/ency/imagepages/19465.htm
- Morse, J. M., Morse, R.M., & Tylko, S.J. (1989). Development of a scale to identify the fall-prone patient. Canadian Journal on Aging, 8(4), 366-377.
- Naqvi, U. & Sherman, A. I. (2020). Muscle strength grading. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436008/ Accessed July 15, 2021
- Vilella, R.C. & Reddivari, A. (2020). Musculoskeletal examination. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK551505/ Accessed July 15, 2021.
- “Neuro Exam Image 41.png” and “Neuro Exam Image 39.jpg” by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0
- “Musculoskeletal Exam Image 2.png,” “Neuro Exam image 6.png,” and “Musculoskeletal Exam Image 7.png” by Meredith Pomietlo for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵

