10 Focused Assessment – Cardiovascular System
Learning Objectives
At the end of this chapter, the learner will:
- Obtain health history related to the heart and peripheral vascular systems.
- Perform physical assessment of the heart and the peripheral vascular system using correct techniques.
- Document findings of cardiac and peripheral-vascular assessment.
I. Overview of the Cardiovascular System
The assessment of the cardiovascular system will include examinations of the peripheral vascular system by assessing color, temperature, edema, capillary refills, and peripheral pulses, as well as examinations of the heart by inspecting, palpating, and auscultating its landmarks.
II. Anatomy and Physiology
Click the link below to review the anatomy and physiology of the circulatory system. During the assessment process, you will need to apply your knowledge of A & P to the heart and peripheral vascular system.
Knowledge Check
III. Medical Terminology
| Angina pectoris | chest pain, a result of myocardial ischemia |
| Arteriosclerosis (Atherosclerosis) | formation of plaques of fatty material within arterial walls |
| Bradycardia | slow heart rate |
| Bruit | a blowing sound heard in auscultation over a peripheral vessel or an organ. |
| Capillary Refill Time (CRT) | time required for return of color after application of blanching pressure to a distal capillary bed |
| Cyanosis | bluish-gray discoloration of the skin |
| Diastole | period of time within the cardiac cycle in which ventricles are relaxed |
| Ecchymosis | discoloration of skin caused by leakage of blood into the subcutaneous tissue |
| Embolus | blood clot or foreign object in the circulatory system |
| Heart murmurs | a blowing, whooshing, or rasping sound heard during a heartbeat which is caused byturbulent blood flow through the heart valves or near the heart |
| Hypertension | high blood pressure |
| Korotkoff Sounds | series of sounds that correspond to changes in blood flow through an artery as pressure is released |
| Myocardial infarction | heart attack |
| Palpitations | sensations of pounding or racing of the heart |
| Pitting Edema | an indentation remains after the swollen skin is pressed |
| Point of Maximal Impulse (PMI) | corresponds to the left ventricular apex of the heart, which can be palpated in the fifth intercostal space at the midcalvicular line |
| Pulse Pressure | difference between systolic and diastolic pressure |
| Prehypertension | an elevated systolic blood pressure of 120-139 mmHg and diastolic 80-89 mmHg |
| Syncope | temporary loss of consciousness resulting from decreased perfusion to the brain, which can be due to reduced cardiac output |
| Systole | period of time within the cardiac cycle in which ventricles contract |
| Tachycardia | rapid heart rate |
| Thrills | vibratory sensations felt on the skin overlying the heart, which can be detected in loud murmurs |
| Thrombus | blood clot |
| Deep Venous Thrombosis (DVT) | formation of a blood clot in a deep vein |
Knowledge Check
IV. Step by Step Assessment
- Perform hand hygiene.
- Check room for contact precautions.
- Introduce yourself to patient.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain process to patient.
- Assemble equipment prior to starting exam.
- Be organized and systematic in your assessment.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure patient’s privacy and dignity.
- Apply principles of asepsis and safety.
- Check vital signs.
| Steps |
Additional Information |
| 1. Conduct a focused interview related to cardiovascular and peripheral vascular disease. | Ask relevant questions related to chest pain, palpitations, shortness of breath (dyspnea), cough, edema, fatigue, leg pain, skin changes, and swelling in limbs.
Review medical history for past illnesses such as diabetes, hypertension, high cholesterol. Review the family history of heart problems, hypertension, diabetes, and high cholesterol. Assess the social history, including smoking, exercise habits, and alcohol consumption. |
|
2. Inspect:
|
Cyanosis is an indication of decreased perfusion and oxygenation.
Alterations and bilateral inconsistencies in CWMS may indicate underlying conditions or injury. While checking for capillary refill, inspect the nail base angle. The normal angle of the nail base is 160 degrees. Assessing for Clubbing Fingers However, if the angle of nails become greater than 160 degrees, they are called clubbing fingers. Clubbing fingers are related to chronic hypoxemia.  Sudden onset of intense, sharp muscle pain that increases with dorsiflexion of foot is an indication of DVT, as is increased warmth, redness, tenderness, and swelling in the calf.  Note: DVT requires emergency referral because of the risk of developing a pulmonary embolism. |
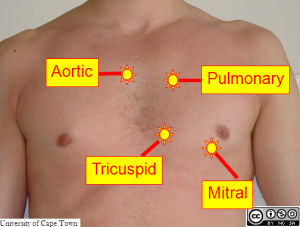
| 3. Auscultate:
Have the patent breathe normally. Use the diaphragm side of the stethoscope to hear the five landmark areas:
|
Aortic Area – 2nd ICS on the right sternal border.
Pulmonic Area – 2nd left ICS ERB’s Point – 3rd left ICS Tricuspid Area – 4th left ICS (for children 4th or 5th left ICS) Mitral Area (Apical) – 5th left ICS medial to the MCL
Auscultate for rate, rhythm, and pitch (the quality of the sound). Auscultate apical pulse at the fifth intercostal space and midclavicular line. Note the heart rate and rhythm. Identify S1 and S2 and follow up on any unusual findings. |
4. Palpate:
Locations of Pulsation Sites:
|
Pulse Amplitude (strength): 0 = absent; 1+ = decreased, barely palpable; 2+ = normal; 3+ = Full volume; 4+ = bounding pulse Absence of pulse may indicate vessel constriction, possibly due to surgical procedures, injury, or obstruction.
|
| 5. Report and document assessment findings and related health problems according to agency policy. | Accurate and timely documentation and reporting promote patient safety. |
Note: Click all hyperlinks to access more details. Copyrighted materials used with permission of the author, A. Chandrasekhar, Loyola University Medical Education Network.
V. Documentation of Assessment Findings
A sample of the narrative documentation:
A & Ox4, patient appears comfortable in bed. Chest is symmetrical expansion with respiration, no scars. No cardiac heaves or lifts. No thrills is palpated. PMI noted at fifth intercostal space and midclavicular line. Normal S1 and S2 with regular rate and rhythm. No rashes, swelling, color change, or cyanosis in arms or legs. No clubbing in fingernails. Capillary refill is < 2 sec. Hands and feet pink and warm to touch. No pitting edema in feet.
VI. Related Laboratory and Diagnostic Procedures/Findings
Some blood tests related to the cardiovascular system are frequently used, such as cholesterol tests, which measure the levels of fat and cholesterol in the bloodstream. When serum cholesterol levels are high, the patient is at increased risk for cardiovascular problems. If there is an abnormal finding in the physical assessment, the patient may need additional diagnostic procedures to further identify potential cardiovascular disease. These diagnostic cardiac tests can be non-invasive, such as:
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart.
- Holter Monitoring (or Ambulatory ECG): Records the electrical activity during daily activities.
- Chest X-ray: Examines the size of the heart.
- Echocardiogram: Uses high-frequency sound waves to view the size, structure, and motion of the heart.
- Exercise stress test (or Treadmill test): Examines the heart function while exercising on a treadmill.
Diagnostic tests can also be invasive, such as:
- Cardiac Catheterization or Coronary Angiogram: Checks for heart abnormalities or coronary artery problems.
A more detailed overview of different cardiac diagnostic tests is available at: Cardiac Diagnostic Tests
VII. Learning Exercises
VIII. Attributions and References
- Busti, A. J. Pitting edema assessment. EBM Consult. September 2016. DOI: https://www.ebmconsult.com/articles/pitting-edema-assessment
- Chandrasekhar, A. Screening physical exam. March 2006. http://www.meddean.luc.edu/lumen/MedEd/medicine/pulmonar/pd/pstep75.htm
- Desherinka. File:Acopaquia.jpg. (2014, March 4). Wikimedia Commons, the free media repository. Retrieved 23:54, August 29, 2019 from https://commons.wikimedia.org/w/index.php?title=File:Acopaquia.jpg&oldid=118072980.
- Doyle, G. R. & McCutcheon, J. A. Step by Step Checklist adapted from https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/
- Gibson, M. & Zorkun, C. Heart sounds. June 2015. DOI: https://www.wikidoc.org/index.php/Heart_sounds
- Khan Academy: Circulatory system and the heart by Sal Khan. https://www.khanacademy.org/science/health-and-medicine/circulatory-system/circulatory-system-introduction/v/circulatory-system-and-the-heart
- MedlinePlus. Cardiac diagnostic tests. US National Library of Medicine. DOI: https://medlineplus.gov/hearthealthtests.html
- Textbook of Cardiology. Physical examination. December 2012. DOI: https://www.textbookofcardiology.org/wiki/Physical_Examination%23Cardiac_Auscultation