5 Documentation of Health Assessment Findings
Learning Objectives
At the end of this chapter, the learner will:
1) document assessment findings using best practice standards
2) recognize variations in the documentation of assessment findings ( paper. electronic)
3) evaluate the legal implications of accurate and concise documentation in nursing practice.
I. Overview of Documentation of Assessment Findings
In the article Nursing record systems: effects on nursing practice and healthcare outcomes by Urquhart C, Currell R, Grant MJ, Hardiker NR nurses document to record the care that was planned, any deviations, and the actual care given to each patient by the registered nurse (RN) or any caregivers working with the RN to provide patient care. The article further states that documentation should demonstrate the legality of the care given and should be professionally completed. Legally only actions or care documented are seen as being completed. This sentiment is reflected by the nurse’s mantra of “If it was not documented, it was not done.” It is important that these rules apply to written documentation in the physical chart and electronic charting (EHR). Other aspects of documentation include the importance of documenting in a timely manner, avoiding using abbreviations, and writing the note in grammar-appropriate standard English. Remember, if the note goes to court it is important that the jury can read it grammatically and legibly.
Documentation is used for:
- creating plans of care.
- communicate findings
- ensuring continuity of care across shifts.
- proof of education given
- monitoring quality assurance.
- obtaining reimbursement by insurance, Medicare, and Medicaid.
- research and research-based interventions
- Discharge concerns/readiness-homecare needs
- legal concerns.
The primary care provider (MD, NP, PA), consulting physicians, social worker, Physical therapist, occupational therapist, nutritionist, and possibly the clinical pharmacist all use the progress note section to document. Nurses use the “Nurse’s Notes” or the progress note section to communicate therefore, it is important that the nurse read the physical or electronic progress note to determine the patient’s course of care and possible discharge dates.
Seven criteria for nursing documentation were presented in 2010 by Jefferies, Johnson, and Griffiths (2010:119) in the paper: “A meta-study of the essentials of quality nursing documentation.” The seven criteria for professional and legal documentation include Patient-centered, contain the nursing care given, reflect the nurses’ clinical judgment, is presented in a logical order, written in real-time, document variance in the patient’s care, and fulfill the legal requirements. The nurse needs to document significant events and information in any patient’s ongoing care from assessment, planning, intervention, and evaluation. Documentation facilitates safety and quality care in so many ways, one of which is the continuity of care from one practitioner to the other. There are also ethical, legal, and financial implications of correct and accurate documentation. Lastly, the literature indicates that nursing documentation can be an indicator of quality nursing practice and patient mortality.
All types of documentation must have the date, time, and signature of the person documenting.
Knowledge Check
II. When does the nurse document?
- At admission to a unit or procedure
- When accepting a transfer or sending a transfer to another floor.
- After the head to toe assessment
- After a focused assessment when a change in patient status has been noticed.
- After medication administration, especially after the administration of pain medication.
- After any teaching is given.
- After any wound inspection or wound dressing change.
- Progress notes every two hours, after a change in patient status, after an emergency, or at the end of a shift depending on the hospital policy.
- At the occurrence of significant events.
III. The nurse may use different types of documentation.
The type used is normally mandated by the hospital and may be different in the critical care areas of the Emergency Department, the Intensive Care Units, Hemodialysis and Psychology. The most commonly used types are listed here:
- Charting by Exception: Only the abnormal findings on an assessment are recorded and it is also used to document communication with other health care providers.
- Focused DAR Notes which can be used with the Charting by Exception note:
- D for Data: All assessment findings plus vital signs. The data section corresponds with the assessment portion of the nursing process.
- A for Action: All nursing actions and incorporates the planning and implementation stages of the nursing process.
- R for Response: this section documents the patient’s response to the nurse’s action and evaluates if the nurse’s action (intervention) worked or not. This incorporates the Evaluation phase of the nursing process.
-
- View sample charting by exception paper documentation with associated DAR notes for abnormal findings. Please click on the link and open it in a new window to see the example.
- For more information about writing DAR notes, visit What is F-DAR Charting?
The third type of note is the Narrative note:
- Narrative Notes are a type of progress notes that give a short snapshot of the patient’s status, assessment findings, nursing activities, and care given at certain chronological intervals during the entire shift. Please use this link Guide to Documentation for Nurses to see examples of the Narrative note.
The fourth type of note is the SOAPIE:
- SOAPIE is a mnemonic for a type of progress note that is organized into six categories: Subjective, Objective, Assessment, Plan, Interventions, and Evaluation. SOAPIE progress notes are written by nurses, as well as other members of the health care team.
- Subjective: This section includes what the patient said, such as, “I have a headache.” It can also contain information related to pertinent medical history and why the patient is in need of care.
- Objective: This section contains the observable and measurable data collected during a patient assessment, such as the vital signs, physical examination findings, and lab/diagnostic test results.
- Assessment: This section contains the interpretation of what was noted in the Subjective and Objective sections, such as a nursing diagnosis in a nursing progress note or the medical diagnosis in a progress note written by a health care provider.
- Plan: This section outlines the plan of care based on the Assessment section, including goals and planned interventions.
- Interventions: This section describes the actions implemented.
- Evaluation: This section describes the patient’s response to interventions and if the planned outcomes were met.
The fifth type of note is the Patient Discharge Summary:
- When a patient is discharged from an agency, a discharge summary is documented in the patient record, along with clear verbal and written patient education and instructions provided to the patient. Discharge summary information is frequently provided in a checklist format to ensure accuracy and includes the following:
- Time of departure and method of transportation out of the hospital (e.g., wheelchair)
- Name and relationship of the person accompanying the patient at discharge
- Condition of the patient at discharge
- Patient education completed and associated educational materials or other information provided to the patient
- Discharge instructions on medications, treatments, diet, and activity
- Follow-up appointments or referrals given
The sixth type of documentation is the Minimum Data set (MDS) Charting
Minimum Data Set (MDS) Charting
In long-term care settings, additional documentation is used to provide information for reimbursement by private insurance, Medicare, and Medicaid. The Resident Assessment Instrument Minimum Data Set (MDS) is a federally mandated assessment tool created by registered nurses in skilled nursing facilities to track a patient’s goal achievement, as well as to coordinate the efforts of the health care team to optimize the resident’s quality of care and quality of life. This tool also guides nursing care plan development.
-
- Read more details about MDS charting in the Long-Term Care Facility Resident Assessment User Manual established by the Centers for Medicare and Medicaid Services (CMS).
- Review the information through the link below: ( note: the word resident refers to patients )
Knowledge Checl
IV. Another resource is the Guide to documentation for Nurses
The link above gives a great review of what was discussed above, more samples of narrative documentation, samples of documentation flow sheets, and discusses documentation and the state law (Texas). Please remember that each state has a Nursing Board of Licensure which maintains a state-specific Nursing Practice Act.
V. The most commonly used type of documentation used now is electronic documentation.
The same rules apply but the medium has changed from paper to computer:
In today’s health care environment, all the information in the prior guide must also be applied to electronic health records management.
The EHR for each patient contains a great deal of information. The most frequent pieces of information that nurses access include the following:
- History and Physical (H&P): A history and physical (H&P) is a specific type of documentation created by the health care provider when the patient is admitted to the facility. An H&P includes important information about the patient’s current status, medical history, and the treatment plan in a concise format that is helpful for the nurse to review. Information typically includes the reason for admission, health history, surgical history, allergies, current medications, physical examination findings, medical diagnoses, and the treatment plan.
- Provider orders: This section includes the prescriptions, or medical orders, that the nurse must legally implement or appropriately communicate according to agency policy if not implemented.
- Medication Administration Records (MARs): Medications are charted through electronic medication administration records (MARs). These records interface the medication orders from providers with pharmacists and are also the location where nurses document medications administered.
- Treatment Administration Records (TARs): In many facilities, treatments are documented on a treatment administration record.
- Laboratory results: This section includes results from blood work and other tests performed in the lab.
- Diagnostic test results: This section includes results from diagnostic tests ordered by the provider such as X-rays, ultrasounds, etc.
- Progress notes: This section contains notes created by nurses and other health care providers regarding patient care. It is helpful for the nurse to review daily progress notes by all team members to ensure continuity of care.
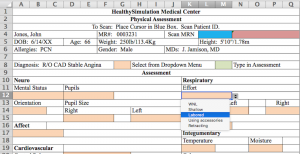
VI. A sample of an electronic health record (EHR) Physical Assessment Document
A nursing note sample
Here is a sample of an Electronic Health Record of a Physical Assessment
A more detailed overview of what and how to document. Please click the link below:
VI: Learning Activity:
VI. Citations and Attributions
Urquhart C, Currell R, Grant MJ, Hardiker NR. Nursing record systems: effects on nursing practice and healthcare outcomes. Cochrane Data Base Syst Rev. 2009;1:1–66.
Tasew, H., Mariye, T. & Teklay, G. Nursing documentation practice and associated factors among nurses in public hospitals, Tigray, Ethiopia. BMC Res Notes 12, 612 (2019). https://doi.org/10.1186/s13104-019-4661-x
2.5 Documentation Open REsources for Nursing (open RN) by Wisconsin Technical College system Retrieved 13:35 July 27, 2021 https://wtcs.pressbooks.pub/nursingfundamentals/chapter/2-5-documentation/
OKAISU, Elisha M.; KALIKWANI, Florence; WANYANA, Grace and COETZEE, Minette. Improving the quality of nursing documentation: An action research project. Curationis [online]. 2014, vol.37, n.2 [cited 2021-07-27], pp.1-11. Available from: <http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S2223-62792014000200007&lng=en&nrm=iso>. ISSN 2223-6279. http://dx.doi.org/10.4102/curationis.v37i1.1251.
Jefferies, D., Johnson, M. & Griffiths, R., 2010, ‘A meta-study of the essentials of quality nursing documentation’, International Journal of Nursing Practice 16, 112-124. http://dx.doi.org/10.1111/j.1440-172X.2009.01815.x [ Links ]
KAISU, Elisha M.; KALIKWANI, Florence; WANYANA, Grace and COETZEE, Minette. Improving the quality of nursing documentation: An action research project. Curationis [online]. 2014, vol.37, n.2 [cited 2021-07-27], pp.1-11. Available from: <http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S2223-62792014000200007&lng=en&nrm=iso>. ISSN 2223-6279. http://dx.doi.org/10.4102/curationis.v37i1.1251.
Discharge Teaching College & Association of Registered Nurses of Alberta uploaded May 21, 2019. Retrieved 17:30 July 27, 2021, https://youtu.be/J9SGNjrm2Ws
Documentation by the Nurse-Texas Health and Human Services Commission Uploaded September 2016 Wikipedia, Retrieved July 25 2019 https://www.hhs.texas.gov/sites/default/files/documents/doing-business-with-hhs/provider-portal/QMP/NurseDocumentationPPT.pdf
EHR Physical Assessment Document for Simulation – Includes Excel Template by Healthy Simulation Updated July 02, 2020, Retrieved 18:34 July 27, 2021 https://www.healthysimulation.com/14886/ehr-physical-assessment-document-for-simulation-includes-excel-template/
- HealthIT.gov. (2019, September 10). What is an electronic health record (EHR)? https://www.healthit.gov/faq/what-electronic-health-record-ehr ↵
- “Winn_Army_Community_Hospital_Pharmacy_Stays_Online_During_Power_Outage.jpg” by Flickr user MC4 Army is licensed under CC BY 2.0 ↵
- RegisteredNurseRN. (2015, October 16). Charting for nurses | How to understand a patient’s chart as a nursing student or new nurse. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/lNwRvKaNsGc ↵
- RegisteredNurseRN. (2015, October 27). FDAR for nurses | How to chart in F-DAR format with examples. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/BXf7wj9Wmfc ↵
- “1934626790-huge.jpg” by TommyStockProject is used under license from Shutterstock.com ↵
- Centers for Medicare & Medicaid Services. (2019, October). Long-term care facility resident assessment instrument 3.0 user’s manual. https://downloads.cms.gov/files/mds-3.0-rai-manual-v1.17.1_october_2019.pdf ↵

