Communication:Conflict Resolution
Learning Objectives
At the end of this chapter, the learner will:
- Demonstrate effective professional communication to communicate intra and interprofessionally in diverse healthcare settings.
- Demonstrate effective communication techniques in difficult conversations in the workplace.
- Identify strategies used to resolve conflict in the workplace.
Within the context of health care, interprofessional communication can be defined as communication among members of a client care team, which may include members of various professional groups. For example, it may involve you as the nurse, clients, families, and also other healthcare professionals such as physicians, physiotherapists, midwives, pharmacists, dieticians, and personal support workers.

Figure 1: Interprofessional communication
A. Verbal communication may include conversations between two or more members of the interprofessional team, usually in person as illustrated in Figure 1 or over the telephone. See Table 4 for specific communication types and examples that are common in healthcare.
B. Written communication in the interprofessional context commonly includes documentation notes in a client’s chart such as progress notes, physician orders, medication administration record, diagnostic reports, referral letters, and discharge notes. Other examples may include faxes and emails, and more recently, texts.
C. Non-verbal communication in the interprofessional context involves meaning and interpretation conveyed through body language such as facial expressions, eye contact, body position, and gestures. It is important to be aware of your body language and ensure that it aligns with your verbal language.
Table 1: Examples of interprofessional communication
|
Communication type |
Verbal communication example |
|
Client/unit rounds where an interprofessional group discuss the client’s status and plan of care – many times the client and family are involved in these rounds. |
Nurse: “Mr. Molina’s blood pressure has been stabilized all night with no chest pain since 2330. He remains on a saline drip and is scheduled for a cardiac catheterization this morning.” Physician: “What’s his cognitive and renal status like?” Nurse: “He is alert and oriented. No renal issues. He was started on an oral beta blocker last night and had a dose this morning, and was given a dose of 20 mg furosemide this morning too. However, he is wondering about whether he should be restarted on his cholesterol medication.” Physician: “Yes, that is fine to restart, and please notify me when his cath results come back.” Nurse: “Sounds good.” |
|
In-person or phone conversations in which you are providing a client update and consulting another healthcare professional on a plan of action. |
Nurse: “Hello, I am Rita Lin, a registered nurse working with the client Meaka Lorne at General Highschool. Meaka is having suicidal ideation although she does not have an immediate plan. However, I think it is time to initiate more intensive therapy.” Therapist: “Yes, I remember Meaka. How is her anxiety and depression?” Nurse: “Her anxiety has been exacerbated over the last couple of weeks, and as a result she hasn’t been going to school. She has felt quite sad and gloomy over the last week, which is when the thoughts of suicide emerged.” Therapist: “I recall this is how it began last year.” Nurse: “Yes, she also indicated that.” Therapist: “Can you remind me whether she still lives with her father.” Nurse: “Yes, she does, and he is with her at home right now.” Therapist: “Okay, let’s get her in for an appointment.” |
|
Discussions that occur among healthcare professionals while providing client care. |
Physician: “I am just about to insert the central venous catheter, could you shift the light a little this way.” Nurse: “Yes, no problem. I have the IV primed, just let me know when you want me to hand it to you.” Physician: “Will do. Ms. Bykov, you will feel a slight pinch, if you can stay still.” Client: “Okay.” |
Exercises : Check Your Understanding
II. Interprofessional Collaboration
In the USA, The IPEC Core Competencies (CC) have helped to frame the national dialogue on the need for interprofessional education (IPE) and collaborative practice (CP) as a catalyst for improving team-based patient care and enhancing population health outcomes. Interprofessional competencies are inherently linked to patient safety and quality of care and are necessary components of the education of a health professional. Please read this document for more detailed information: Interprofessional Competencies
Interprofessional communication is a fundamental component of interprofessional collaboration. Effective interprofessional collaboration fosters effective teamwork among members of an interprofessional client care team to optimize client outcomes ensuring that clients are safe throughout the healthcare system (Canadian Nurses Association, n.d.a.).
Because of the significance of interprofessional collaboration, the Canadian Interprofessional Health Collaborative has developed a National Interprofessional Competency Framework, as shown in Figure 2.
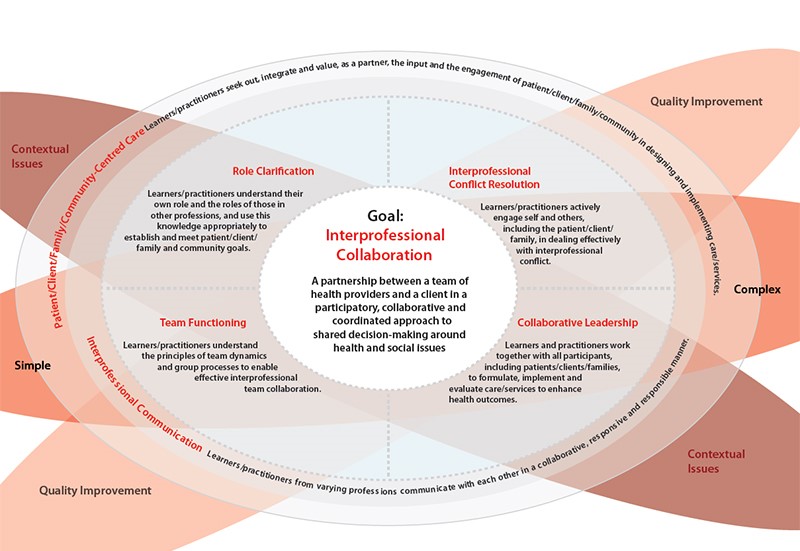
Figure 2: National Interprofessional Competency Framework
As shown in Figure 4.2, six interdependent competency domains have been identified to achieve the goal of interprofessional collaboration. These are defined as the “knowledge, skills, attitudes, and values that shape the judgements essential for interprofessional practice” (Canadian Interprofessional Health Collaborative, 2010, pg. 9) and include:
- Interprofessional communication
- Patient/client/family/community-centered care
- Role clarification
- Team functioning
- Interprofessional conflict resolution
- Collaborative leadership
The first two competencies have a strong influencing role in all healthcare situations, so as shown in the figure, they encircle the other four competencies. This framework can assist you in contributing to effective healthcare team functioning with a focus on communication and working together collaboratively.
This chapter focuses specifically on the competency domain of interprofessional communication. This plays a central role in interprofessional collaboration because it supports the other five competency domains. To fulfill the interprofessional communication competency, nurses and all healthcare professionals must develop the capacity to “communicate with each other in a collaborative, responsive and responsible manner” (Canadian Interprofessional Health Collaborative, 2010, p. 16). This means that each healthcare professional is responsible for engaging in effective communication in the specific clinical and interprofessional context in respectful, explicit, and clear ways (Lyndon et al., 2011).
Consistent execution of successful communication requires attentive listening skills, administrative support, and collective commitment (Lyndon et al., 2011). Other principles of interprofessional communication include:
- Speak clearly with appropriate vocal intonation and at a moderate pace.
- Use simple and clear language.
- Maintain eye contact and show confidence in what you are saying.
- Be efficient in your communication.
- Incorporate adequate, relevant, and timely information.
- Engage in active listening and ask questions for clarification.
- Speak up and seek clarification if needed until your concern regarding a client is addressed.
- Put clients first: always remember – and if appropriate, remind your interprofessional team members – that your decisions and actions affect the client and the client should be the focus of your discussions.
- Show respect in your communication patterns.
Exercises : Check Your Understanding
III. Factors Influencing Interprofessional Communication
There are several factors that can influence interprofessional communication in positive or negative ways – and can therefore have positive or negative effects on healthcare professionals and client outcomes.
The factors affecting interprofessional communication can be divided into three main categories: those related to the physical environment, those related to the context, and those related to communication styles of the people involved. See Figure 4.
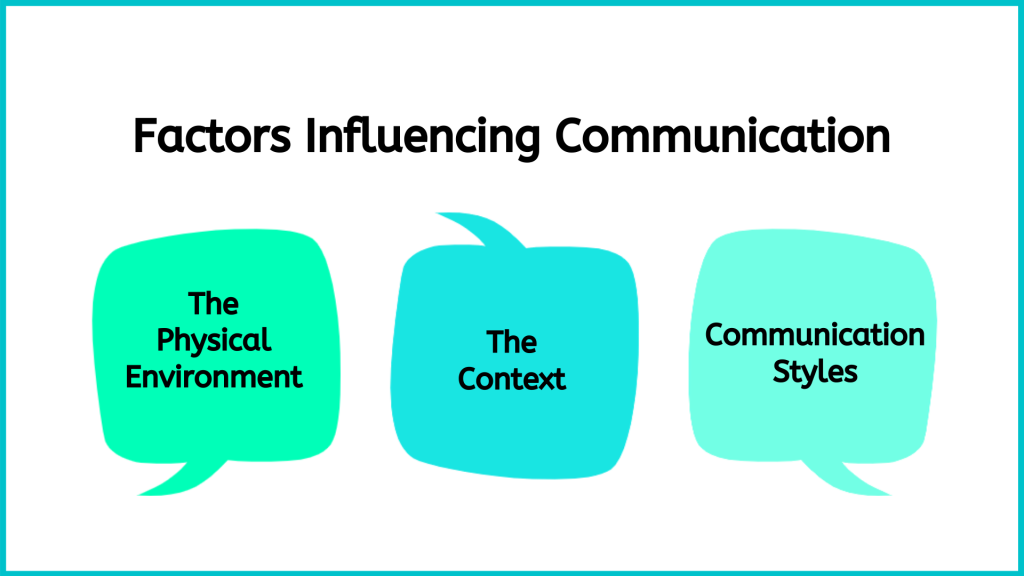
Figure 4: Factors affecting interprofessional communication
You should consider these factors and how you can modify your communication patterns to engage in effective interprofessional communication.
- First, you will often be working in physical environments that are sometimes noisy and have many moving parts including clients, families, and multiple members of interprofessional teams. In addition to the many people, there may be beeping machines and overhead announcements. You should be aware that this can cause sensory overload: healthcare environments are often unfamiliar for clients and their families, so you should take this into consideration.
- Second, interprofessional communication in healthcare environments takes place in a complex context involving a lot of information and dynamic and complex clinical situations that require a high level of acuity. It can be very intense, with life-threatening conditions, death, uncertainty, fear, and anxiety – and can lead to work overload. This context can also influence the dynamic nature and intensity of interprofessional conversations. The hierarchical relationships that exist in interprofessional teams and imbalances of power or ideas about power can also affect how individuals communicate and interpret conversations. It is vital that you communicate clearly, compassionately, and systematically.
- Third, each group of healthcare professionals has their own culture and communication styles, which may not align with those of other healthcare professionals. For example, nurses are often taught to be descriptive and embed narrative elements in their communication. This descriptive style capitalizes on a comprehensive and storied approach. Other healthcare professionals, such as physicians and pharmacists, are taught to be more concise and efficient. As you can imagine, these two communication styles may not always align, so you should reflect on how to tailor your communication to the person or group that you are speaking with, while still communicating your point of view as a nurse.
Table 3 presents examples of ineffective interprofessional communication and strategies to manage each one.
Table 3: Ineffective communication
*HCP = healthcare professional
|
Example |
Effects |
How to manage this type of communication |
|
Disrespectful communication HCP #1 says HCP #1: “It’s 11 am already!” [shakes head in disapproval] “Goodness gracious, you haven’t got her out of bed yet?! What’s wrong with you?”
|
Demoralizes and demeans another person. Although there may be a reason why the client was not helped out of bed, the healthcare professional may feel disempowered and not share the information.
|
HCP #2 could respond by saying: “It is probably better for you to inquire about the reasons that I have not got the client out of bed. Your communication is disrespectful and disregards what is going on with Mrs. Hart. Would you like to know what is going on?” Alternatively, HCP #1, who was initially disrespectful, could have engaged in discussion that is guided by inquiry instead of blame, and said: “I noticed Mrs. Hart is not out of bed yet. How can I help?”
|
|
Example |
Effects |
How to manage this type of communication |
|
Failure to communicate concern. HCP #1: “The client’s BP is 140/88” HCP #2: “Okay.”
|
The first healthcare professional stated a finding, but did not indicate or emphasize their concern. Thus, the second healthcare professional did not recognize the need to be concerned or engage in a dialogue. Failure to communicate one’s concern can have a negative effect on patient outcomes. |
When communicating, it is important to explicate and emphasize when you have concerns and make sure that the individual that you are discussing it with recognizes the importance of what you are saying. For example, the conversation could be modified such that the concern is acknowledged, and they engage in a discussion about the plan of care: HCP #1: “The client’s BP is 140/88. This is out of the ordinary for this client, their baseline BP is 100/60. I have a serious concern about the high BP and I think we should intervene.” HCP #2: “That is quite a jump. Is the client’s pain well-controlled?”
|
|
Example |
Effects |
How to manage this type of communication |
|
Failure to communicate rationale for an action or decision. HCP #1: “Let’s try putting the client in prone position.” HCP #2: “You want us to roll the client onto their abdomen.” HCP #1: “Yes.” HCP #2: “I think that will be difficult.”
|
The communication is not dialogical because of the failure to communicate a rationale for an action or decision by either of these professionals. As a result, neither professional understands the perspective of the other. |
When communicating, it is important to provide rationale for your actions and decisions. For example, the conversation could be modified so that a person’s rationale is clearly identified, as such: HCP #1: “Let’s try putting the client in prone position. Some recent research has suggested that this can improve respiratory function when a client has severe respiratory distress that is not responding to other interventions.” HCP #2: “I am concerned about rolling the client onto their abdomen with all of the tubes and wires. Do you have a suggestion?” HCP #1: “If you are open to it, I can grab one more person and we can do it as a team. What do you think?”
|
|
Example |
Effects |
How to manage this type of communication |
|
Unclear/incomplete communication or miscommunication. HCP #1: “Can you help Ms. Di Lallo with her breakfast?” HCP#2: “Yes” HCP#1: “She’s at table 1.” HCP#2: [walks over to the client], “Hi Ms. Di Lallo, are you ready for your breakfast?” Client: “Yes, can you please pass me my coffee?” HCP#2: [passes Ms. Di Lallo her coffee]. HCP#3: “Oh, hold on! Ms. Di Lallo, we need to thicken your coffee first.”
|
This unclear communication about the client’s diet led to a near miss. Unclear, incomplete, or miscommunication can result in errors related to client care and can have serious consequences for their health. |
When communicating, it is important to include all pertinent information to provide safe, effective care. All healthcare professionals need to clarify any communication shared. For example, the conversation could be modified by ensuring communicating all required information: HCP#1: “Can you help Ms. Di Lallo with her breakfast?” HCP#2: “Yes” HCP#1: “Great, she’s at table 1. Ms. Di Lallo has dysphagia, so you need to make sure all her fluids are thickened and follow the dysphagia diet protocol. The thickener should be on her tray. Do you have any questions?” HCP#1: “No, I’m aware of the dysphagia diet protocol and will monitor Ms. Di Lallo during her meal.” |
|
Example |
Effects |
How to manage this type of communication |
|
Ineffective conflict resolution on a plan of care. HCP#1: “Mr. Pink said he does not feel he is ready to be discharged and I agree.” HCP#2: “I think I’m able to determine when Mr. Pink can be discharged considering I’ve been working with him for 6 months and you just met him last week.” HCP#1: “I think we need to talk to the whole team.”
|
The communication is ineffective because the HCPs disagree about the plan of care for the client. They are not focusing on the context of the interprofessional communication and/or explaining their reasoning based on the client’s needs. They are focusing on their own opinions instead of using a client-centered perspective and evidence-informed approach.
|
In the case of a disagreement, HCPs need to effectively explain their reasons in the context of client-centered care and evidence-informed approaches. It’s always important to use effective conflict resolution strategies. For example, the conversation could be modified as: HCP#1: “Mr. Pink said he does not feel he is ready to be discharged. I agree with him because he has no support system in place to help him with his activities of daily living at home.” HCP#2: “I believe he is physically and mentally ready to go home, but you bring up a good point. Let’s put together a plan for home care.” HCP#1: “Great.”
|
Now, you have learned about the factors that positively and negatively influence interprofessional communication. Inevitably, despite healthcare professionals’ best intentions, conflict is common in interprofessional contexts. Let’s examine this next!
IV. Conflicts in an Interprofessional Environment
Conflict can be defined as a state of serious opposition between two or more perspectives that influences thinking and actions. For example, people may disagree because they have different perspectives. However, varying perspectives alone do not lead to conflict: conflict emerges when one individual’s behaviors impede another individual’s interests or goals, resulting in negative emotions such as fear, anger, and frustration (Barki & Hartwick, 2004, as cited in RNAO, 2012).
Conflict Resolution
Teamwork promotes collaboration, enhances client care outcomes, and fosters a positive work environment. It allows team members to pool their skills, knowledge, and expertise to provide comprehensive and holistic care to clients, while also promoting efficiency and saving organizations money. A strong sense of teamwork encourages open communication, mutual support, and shared accountability among team members, leading to improved client safety and team satisfaction.
Conflict is a natural occurrence on teams. It arises when two or more individuals have opposing thoughts, ideas, feelings, perceptions, behaviors, values, opinions, or actions. It is an inevitable part of professional, social, and personal life and can lead to either constructive or destructive consequences. Constructive consequences of conflict include stimulating growth, fostering open and honest communication, increasing group cohesion and commitment to common goals, facilitating understanding and problem-solving, motivating change, and stimulating creativity. On the other hand, conflict can also have destructive consequences, such as producing hostility within a group, fostering rivalry and competition, and creating misperceptions, distrust, and frustration, resulting in group dissatisfaction with the outcome.
For health care teams to be effective, nurses must be skilled in conflict resolution. Conflicts in health care teams can arise due to differences in opinions, communication breakdowns, or varying work styles. When conflicts are left unresolved, they can lead to tension, decreased morale, and compromised client care. Nurse leaders play a crucial role in promoting effective conflict resolution by fostering an environment that encourages respectful dialogue and active listening. In this manner, conflicts can be addressed promptly and constructively. Through mediation and negotiation, a nurse leader can help team members find common ground, reach compromises, and maintain harmonious working relationships. When resolving conflict, the desired goal is for both parties to reach a satisfactory resolution, known as a “win-win solution.” However, it is important to recognize that a win-win solution is not always possible in every situation.
To address conflicts effectively, various strategies can be employed
- Open communication: Leaders make communication among team members a two-way process where individuals express their thoughts, feelings, and concerns while also actively listening to the thoughts, feelings, and concerns of others.
- Assertive communication: Leaders encourage team members to express themselves in direct, honest, and appropriate ways that also respect the rights of others.
- Respectful communication: Leaders encourage team members to communicate respectfully by maintaining good eye contact, conveying empathy, being aware of nonverbal communication, and focusing on the concern rather than making personal attacks.
By creating a culture of open communication and mutual respect, a nurse leader can improve client outcomes by ensuring that team members work together cohesively, leveraging each other’s strengths, and building on others’ expertise. Moreover, effective conflict resolution allows for the early identification and resolution of issues, preventing conflicts from escalating and negatively impacting the team’s dynamics and client care. Table 1.5 summarizes various conflict resolution approaches.
Table 5. Conflict Resolution Approaches
| Conflict Resolution Approach | Description | Examples |
|---|---|---|
| Collaborative Problem- Solving | Parties work together to find a mutually beneficial solution. | In a health care team, conflict arises between two nurses regarding the fairness of client assignments. They engage in open dialogue, actively listening to each other’s concerns, and collaboratively devise a fair and balanced plan for client assignments based on acuity. View sample dialogue of two nursing participating in collaborative problem-solving. |
| Mediation | A neutral third party facilitates communication and negotiation. | A conflict arises between a nurse and a respiratory therapist regarding a client’s care plan. A nurse manager acts as a mediator, guiding both parties through open communication, helping them understand each other’s perspectives, and reaching a resolution through compromise. View sample dialogue of all parties participating in a mediation approach. |
| Compromising | Both parties make concessions to reach a middle ground. | A conflict arises between two nurses regarding the scheduling of a committee meeting. They compromise by adjusting the meeting time to accommodate both parties’ availability and reach a mutually agreeable solution. View sample dialogue of the two parties participating in a compromise approach. |
| Active Listening and Assertively Communicating | Parties express their concerns and actively listen to each other while also using assertive communication. | Two team members have differing opinions on a client’s treatment plan. They express their concerns assertively, while actively listening to understand each other’s viewpoints, leading to a mutually agreed-upon plan that incorporates the best of both perspectives. View sample dialogue of both parties participating in active listening and assertive communication. |
| Escalating Up the Chain of Command | Parties involve higher-level supervisors to intervene. | A conflict between two health care professionals becomes persistent and unresolvable. The issue is escalated to the department head or supervisor, who intervenes to find a resolution and restore cohesiveness and function within the team. View sample dialogue of parties involved in escalating up the chain of command. |
| Avoiding | Parties ignore or withdraw from a conflict. In the short-term, this may be effective in calming heated emotions. However, if this approach is used chronically, it can damage trust and rapport by signaling a lack of interest or commitment. | A conflict arises between two nurses and becomes heated as they discuss a client’s nursing care plan. They agree to take a “time out” and revisit the discussion at a later time. View sample dialogue of two nurses using avoidance as a temporary conflict management strategy. |
| Accommodating | One party resolves the conflict by “giving in” to the other party. This may be useful when one party realizes they are in error or if the other party is an expert or has more experience. However, it is also crucial to be aware of when accommodating might be detrimental to you or your team’s best interest. | A conflict arises when two nurses disagree on the best way to initiate IV access for a client. View sample dialogue on one nurse who uses an accommodating conflict resolution strategy. |
Exercises:
Consider the following example conflict in a health care setting requiring conflict resolution and reflect on conflict resolution strategies that could be implemented.
Scenario: Conflict Requiring Conflict Resolution
In a long-term care facility, Sarah, an LPN/VN, and Emma, a certified nursing assistant, find themselves in a conflict regarding the delegation of tasks and workload distribution. Sarah believes that Emma is not taking on her fair share of responsibilities or providing adequate support to the residents. On the other hand, Emma feels overwhelmed by the assigned workload and believes that Sarah is not acknowledging her efforts. Both parties firmly believe they are “right” within their positions and are unwilling to compromise.
- What conflict resolution strategy could be used to satisfactorily address the conflict between these two team members?
Exercises
Points of Consideration
Interprofessional communication can be optimized using a client-centered perspective and an evidence-informed approach. It should be guided by discussions that are centered on the client’s wellbeing and incorporate the best possible evidence for each client.
V. Resources to Facilitate Interprofessional Communication
There are numerous resources to facilitate interprofessional collaboration and teams, including interprofessional communication.
Several standardized tools have been developed to facilitate interprofessional communication (Canadian Medical Protective Association, 2011) and prevent and manage harassment, errors in the workplace, and miscommunication. The SBAR tool, and its variations including ISBAR, is one common communication tool that can facilitate effective verbal communication when communicating with another healthcare professional about a client or during handover. It provides a framework so that communication is focused, concise, and complete.
ISBAR, detailed in Figure 4.7, is an acronym for Introduction, Situation, Background, Assessment, Recommendation. It was first introduced by the military in the United States to facilitate communication (NHS Improvement, n.d.) and has since been taken up in the healthcare arena to enhance client safety by facilitating communication among healthcare professionals and ensure the most important information is included (NHS improvement, n.d.; Spooner et al., 2016).
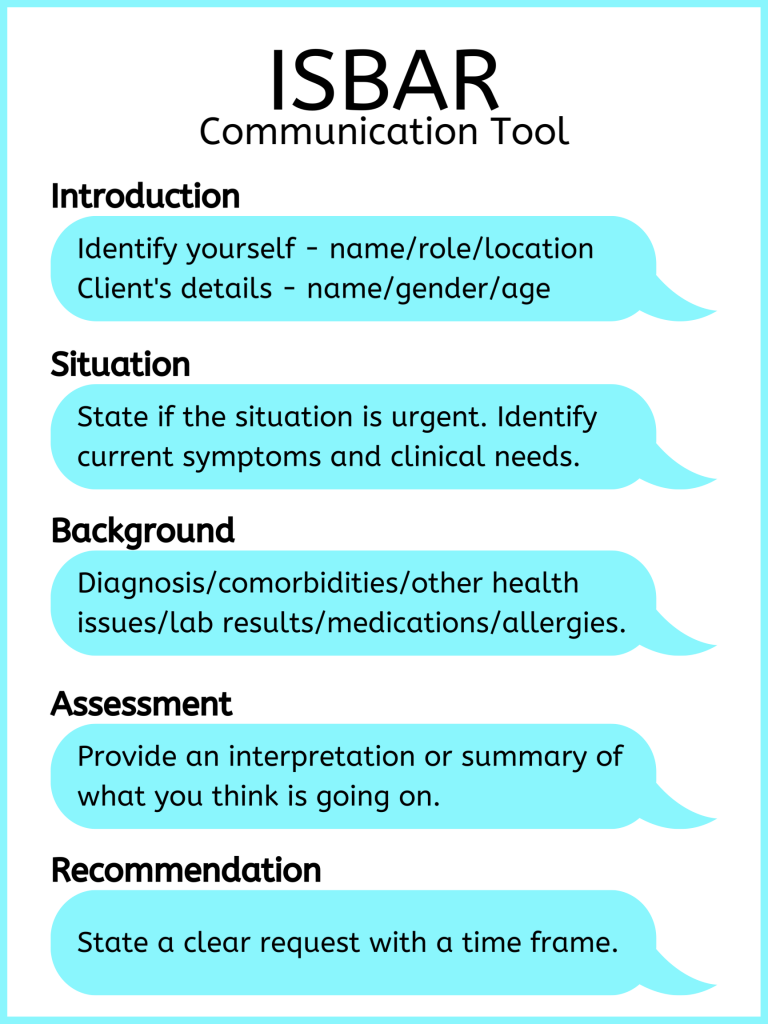
Figure 7: ISBAR
Exercises
Using the ISBAR effectively takes practice.
- Watch the Film Clip 4.1 about ISBAR [3:08].
2. Share your thoughts on this video
Research suggests that nurses do not comprehensively use elements of ISBAR, and the sections on assessment and recommendation are consistently neglected (Spooner et al., 2016). It is important to reflect on how you communicate and how you can improve through comprehensive use of tools. See Table 4.4 for an example of effective use of the ISBAR to guide communication.
Table 4: Example of ISBAR Use
|
I – Introduction
|
“Hello, I am calling about Zina Mills, a 45-year-old female client on 3C. I am Sandu Martique, a registered nurse on the unit.”
|
|
S – Situation
|
“The client is experiencing shortness of breath with a productive cough, and green mucous times three days. Currently, she has moderate crackles throughout the left lobe. 02 sat is 90%, respiratory rate is 26, temp is 38.3, pulse 98, blood pressure 134/88, and she is on 4 litres oxygen via nasal prongs.”
|
|
B – Background
|
“The client has been in this facility for 4 days following hip surgery. Her incisions show no signs of infection. However, her mobility has been limited due to moderate dementia. She has a history of hypertension, no previous lung disease, and is a non-smoker.”
|
|
A – Assessment
|
“Based on my assessment, her symptoms may be associated with pneumonia.”
|
|
R – Recommendation
|
“Would you like a chest x-ray done? And when do you have time to see the client?”
|
COMMUNICATING WITH HEALTH CARE TEAM MEMBERS-ISBARR
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 8 [7] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports.
Nurses routinely report information to other health care team members, as well as urgently contact health care providers to report changes in patient status.
Standardized methods of communication have been developed to ensure that information is exchanged between health care team members in a structured, concise, and accurate manner to ensure safe patient care. One common format used by health care team members to exchange patient information is ISBARR, a mnemonic for the components of Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
-
Introduction: Introduce your name, role, and the agency from which you are calling.
-
Situation: Provide the patient’s name and location, why you are calling, recent vital signs, and the status of the patient.
-
Background: Provide pertinent background information about the patient such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
-
Assessment: Share abnormal assessment findings and your evaluation of the current patient situation.
-
Request/Recommendations: State what you would like the provider to do, such as reassess the patient, order a lab/diagnostic test, prescribe/change medication, etc.
-
Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the patient’s chart.
Read an example of an ISBARR report in the following box. A hyperlink is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear and her heart rate is regular.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
Points of Consideration
Think about what you want to say and how you want to say it before you say it. Organize your thoughts first.
VI. Application in Practice
Exercise: Conflict Resolution
Conflicts often occur in the workplace due to multiple factors that stem from varying goals, miscommunication, personality differences, etc. Inability to navigate conflict can impact both professional and personal lives. It is necessary that learners acquire the skills in “a practice environment”, or reflect through this example:
- Watch and reflect . Share your reflections to the class:
-
- What is the story? Watch this
-
- What thoughts ran through your mind?
- What were the actions/communication techniques displayed by the professionals?
- What are the responses of the team members? Clients?
- What are the desired outcomes? Were they achieved? How/Why?
- If you have to redo the situation, how will it be done in your own practice setting?
Key Takeaways
- Interprofessional communication occurs between members of various professions and can also include the client/family.
- Interprofessional communication is a fundamental component of interprofessional collaboration and optimizing client outcomes.
- Several factors influence interprofessional communication, including the physical environment, context, and communication styles.
- Respectful interprofessional communication and interaction is essential to safe and effective work environments, including healthcare settings.
- ISBAR is a commonly used tool that can facilitate effective communication with other healthcare professionals.
- Awareness of one’s personal communication styles and values helps facilitate interprofessional communication.
VII. Assignment
Assignment Reflections: Nontherapeutic vs therapeutic communication
Submit through blackboard assignment submission link.
I. Watch the video one more time: “Nontherapeutic vs therapeutic communication” https://www.youtube.com/watch?v=Ik_hwMHVHM4
II. Answer the following questions:
- What is the patient concerned about?
- How does the nurse respond to the patient?
- How does the patient react to the nurse’s responses?
- Write a summary of your observations and the implications for the nurse patient relationship.
- Explain How the nurse could effectively communicate with this patient to address her concerns?
Resources:
Communicating with Health Care Team Members: https://batch.libretexts.org/print/url=https://med.libretexts.org/Bookshelves/Nursing/Nursing_Fundamentals_(OpenRN)/02%3A_Communication/2.04%3A_Communicating_with_Health_Care_Team_Members.pdf
Introduction to Documentation https://jcu.pressbooks.pub/nursingdocumentation/chapter/introduction-to-documentation/
Indications for Documentation https://jcu.pressbooks.pub/nursingdocumentation/chapter/indications-for-documentation/
Ethicolegal, Safety and Quality Considerations in Documentation: https://jcu.pressbooks.pub/nursingdocumentation/chapter/ethicolegal-safety-and-quality-considerations-in-documentation/
Documentation Principles: https://jcu.pressbooks.pub/nursingdocumentation/chapter/principles-of-documentation/
Documentation Frameworks; https://jcu.pressbooks.pub/nursingdocumentation/chapter/documentation-frameworks/
Documentation in Nursing: 1st Canadian edition: https://pressbooks.library.torontomu.ca/documentation/front-matter/introduction/
References and Attributes:
- World Health Organization. (2010). Framework for action on interprofessional education & collaborative practice. https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice ↵. [PubMed] [Reference list]
- AHRQ. (2015, July). TeamSTEPPS: National implementation research/evidence base. https://www.ahrq.gov/teamstepps/evidence-base/safety-culture-improvement.html ↵. [Reference list]
- American Association of Colleges of Nursing (2011): Core Competencies for Interprofessional Collaborative Practice https://ipec.memberclicks.net/assets/2011-Original.pdf
- Lapum, J., St-Amant, O., Hughes, M., Garmaise-Yee, J., & Lee, C. (2020). Introduction to communication in nursing.
- NHS Improvement. (n.d.). SBAR communication tool – situation, background, assessment, recommendation. Retrieved from: https://improvement.nhs.uk/documents/2162/sbar-communication-tool.pdf
- Spooner, A., Aitken, L., Corley, A., Fraser, J., & Chaboyer, W. (2016). Nursing team leader handover in the intensive care unit contains diverse and inconsistent content: An observational study. International Journal of Nursing Studies, 61, 165-172.
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association ↵. [Reference list]
- Russotto, J., Tierney, L., & Stype, J. (2019). Conflict resolution strategies used by nurse managers and the impact on the staff nurse. Journal of Nursing Administration, 49(9), 455-461. https://doi.org/10.1097/NNA.0000000000000770 ↵
- Haack, M. R., & Hughes, L. C. (2019). Conflict resolution styles of nurses and their impact on the work environment. Journal of Nursing Management, 27(2), 406-414. https://doi.org/10.1111/jonm.12668 ↵
- Ambrose, M. K., Seabert, D., & Schminke, M. (2021). Conflict management and resolution strategies in healthcare organizations. In Handbook of Conflict Management Research. Edward Elgar Publishing. https://doi.org/10.4337/9781789908294.00020 ↵
- Haack, M. R., & Hughes, L. C. (2019). Conflict resolution styles of nurses and their impact on the work environment. Journal of Nursing Management, 27(2), 406-414. https://doi.org/10.1111/jonm.12668 ↵
- LinkedIn. (2023). What are some common pitfalls or challenges of using an avoiding style in conflict management? https://www.linkedin.com/advice/1/what-some-common-pitfalls-challenges-using-avoiding ↵
- Indeed. (2023). 5 major conflict management styles for managers. https://www.indeed.com/career-advice/career-development/conflict-management ↵


