Week 6: Clinical Judgment Part A
Unit Learning Outcomes
At the end of this chapter, the learner will:
1. Compare and contrast three approaches to problem solving.
2. Describe models of clinical judgment for critical thinking and decision-making judgments.
3. Discuss clinical judgment and decision-making necessary to provide quality care.
Overview of this Chapter
This chapter will introduce the concept of clinical judgement, a vital process where nurses make decisions using their knowledge, clinical reasoning and critical thinking. It is important to understand concepts related to clinical judgement(CJ) in nursing practice. This chapter is the part A of this concept and will include concepts related to clinical judgement, models of CJ and how important it is to provide safe nursing care to patients.
Nurses make decisions while providing patient care by using critical thinking and clinical reasoning . Let’s review what is critical thinking, clinical reasoning and clinical judgement.
Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”[1] Using critical thinking means that nurses take extra steps to maintain patient safety and don’t just “follow orders.” It also means the accuracy of patient information is validated and plans for caring for patients are based on their needs, current clinical practice, and research. “Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized patient concern, and generate the best possible evidence-based solutions in order to deliver safe patient care.” The NCSBN administers the national licensure exam (NCLEX) that measures nursing clinical judgment and decision-making ability of prospective entry-level nurses to assure safe and competent nursing care by licensed nurses.
Exercises: Pre-class:
Watch the video prior to class and be ready to discuss in the class. See the task below the video .
In-class discussion:
Give an example of how you have used critical thinking, decision making & clinical reasoning in everyday life.
I. Clinical Judgment and Nursing
When collecting subjective and objective data, you need to consider clinical judgment. In nursing, the purpose of health assessment is to facilitate clinical judgment, which is defined as:
- A determination about a client’s health and illness status.
- Their health concerns and needs.
- The capacity to engage in their own care.
AND - The decision to intervene/act or not – and if action is required, what action (Tanner, 2006).
The nursing process is the foundation of clinical judgment. However, clinical judgment is more comprehensive, action-oriented, and guided by the philosophy of client safety. Thus, it is important to learn when to act to prevent clinical deterioration, a worsening clinical state related to physiological decompensation (Padilla & Mayo, 2017).
To facilitate clinical judgment, you must determine if the collected data represent normal findings or abnormal finding. When findings are abnormal, you must act on these cues as they signal a potential concern and require action. Failing to recognize abnormal findings and act on these cues can lead to negative consequences including sub-optimal health and wellness – and more importantly, clinical deterioration. Some abnormal findings are considered critical finding that place the client at further risk if the nurse does not act immediately.
The process leading to clinical judgment is described as clinical reasoning. This process involves:
- Thoughtfully considering all client data as a whole, whether each piece of information is relevant or irrelevant, and how each piece of information is related or not related.
- Recognizing and analyzing cues. Is the information collected a normal, abnormal, or critical finding? Can the information be clustered to inform your clinical judgment?
- Interpreting problems. What is the priority problem and what are the factors causing it? What else do you need to assess to validate or invalidate your interpretation? What other information do you need to collect to make an accurate clinical judgment?
- Determining, implementing, and then evaluating appropriate actions (Dickison et al., 2019; Tanner, 2006).

Figure 6.1 Looking for Cues
The clinical reasoning process is encompassed by critical thinking. This means that when engaging in the process of clinical reasoning, you should systematically analyze your own thinking so that the outcomes are clear, rational, creative, and objective with limited risk of judgment and error.
Clinical Judgement
A client tells you “I have a headache.” As the nurse, you immediately recognize the cue: headache. However, you do not have sufficient information to analyze this cue and identify the significance. Thus, you may ask a series of subjective questions such as “When did the headache start? What were you doing when it started? Have you ever had this type of headache before?” The client’s response will provide you detailed information to facilitate your critical thinking and the process of hypothesizing what is going on, and thereby helping you determine what actions to take.
Clinical judgement is facilitated by cognitive steps that help you determine when and how to act to prevent clinical deterioration; see Table 6.1. Like the nursing process, these steps should be performed in an iterative manner as per the client situation and your clinical reasoning process.
Table 6.1: Clinical judgment steps (developed based on NCSBN, 2020)
|
Steps |
Considerations |
|---|---|
|
Recognize cues |
Recognizing cues involves identifying findings that require action because they are abnormal. This involves what Tanner (2006) calls “noticing” (i.e., recognizing when something is abnormal). You should be asking yourself what matters most? |
|
Analyze cues |
Analyzing cues involves interpreting/making sense of the collected data, what it means, and how it may relate to possible pathophysiological processes. This involves what Tanner (2006) calls “interpreting”, making sense of the collected data. |
|
Prioritize hypotheses |
Prioritizing hypotheses involves figuring out where to start and how to prioritize care. This step involves what Tanner (2006) refers to as “responding” to the collected data |
|
Generate solutions |
Generating solutions involves identifying the various options (e.g., actions/interventions) to address the problem or the abnormal findings/cues. This may involve identifying which solutions are indicated/effective, nonessential, unrelated, contraindicated. |
|
Take actions |
Taking actions involves identifying the action that should be taken. Examples of actions are specific but could be related to notifying the physician or nurse practitioner, calling for help, monitoring the client, collecting further data. |
|
Evaluate outcomes |
Evaluating outcomes involves determining if the action taken was effective. It may include identifying outcomes that are considered improved, unchanged, or worsened. |
Exercises: Check Your Understanding
Discussion: Watch the video below and Discuss
II. Priorities of Care
Why is clinical judgment important? How does it guide the provision of care?
Clinical judgment is important to ensure the nurse’s actions are based on the client’s most important needs. Clients often have several needs, and some are more important than others. As such, nurses need to assess and evaluate the priorities of care: what actions are most important to take first, and then what actions can follow. Typically, priority actions are those that prevent clinical deterioration and death.
Exercises: CURE Hierarchy
- The CURE hierarchy has been introduced to help novice nurses better understand how to manage competing patient needs. The CURE hierarchy uses the acronym “CURE” to help guide prioritization based on identifying the differences among Critical needs, Urgent needs, Routine needs, and Extras.
You are the nurse caring for the patients in the following table. For each patient, indicate if this is a “critical,” “urgent,” “routine,” or “extra” need.
| Critical | Urgent | Routine | Extra | |
|---|---|---|---|---|
| Patient exhibits new left-sided facial droop | ||||
| Patient reports 9/10 acute pain and requests PRN pain medication | ||||
| Patient with BP 120/80 and regular heart rate of 68 has scheduled dose of oral amlodipine | ||||
| Patient with insomnia requests a back rub before bedtime | ||||
| Patient has a scheduled dressing change for a pressure ulcer on their coccyx |
||||
| Patient is exhibiting new shortness of breath and altered mental status | ||||
| Patient with fall risk precautions ringing call light for assistance to the restroom for a bowel movement |
2.
III. Maslow’s Hierarchy of Needs
Priorities of care can be determined using several frameworks such as Maslow’s Hierarchy of Needs. For example, at the most basic level, life requires an open airway to breathe, the physiological process of breathing, and the circulation of blood and oxygen throughout the body. Airway, breathing, and circulation are the ABCs, which you might have learned if you have taken a cardiopulmonary resuscitation (CPR) course.
Maslow’s Hierarchy of Needs was developed to consider basic human needs and motivations of healthy individuals (Bouzenita & Wood Boulanouar, 2016; Francis & Kritsonsis, 2006; Gambrel & Cianci, 2003). Although not well known, Maslow’s work was closely influenced by the Blackfoot tribe in Canada (James & Lunday, 2014). One version includes five levels of needs: those related to physiological, safety, love, esteem, and self-actualization (Maslow, 1943), which can help prioritize care in nursing. Figure 6.2 presents one adapted version of Maslow’s Hierarchy.
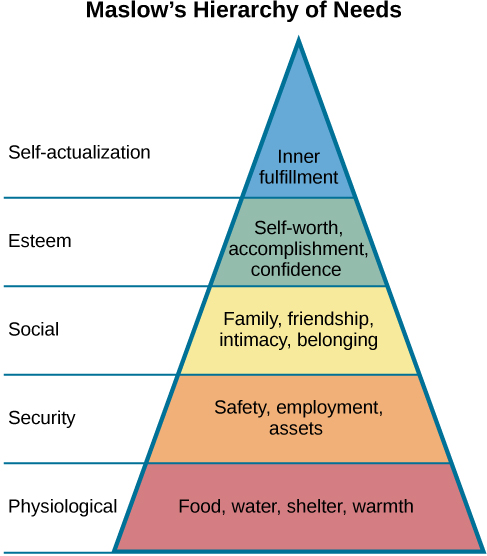
Figure 6.2: Maslow’s Hierarchy of Needs (see attribution statement at bottom of page)
Drawing upon this framework, a nurse can use health assessments to explore five levels of needs:
- Physiological needs – fundamental physical needs required for survival such as air, food/drink, sleep, warmth/clothing/shelter.
- Are these basic physiological needs being met? Is the client’s breathing and circulation supported?
- Safety – needs related to a secure physical and emotional environment.
- Does the client feel safe and secure in general in life? Does the client feel safe and secure in the healthcare environment? Is the bed lowered to the lowest position when you finish your assessment? Is the call bell in reach?
- Love and belongingness – needs related to relationships including friendship and family, intimacy and affection, work, and trust and acceptance.
- Does the client feel love and belongingness in general in their relationships? More specifically, does the client feel cared for by nurses and other healthcare providers?
- Esteem – feelings related to self-worth, dignity, respect, and achievement.
- Does the client feel respected and valued in general by others? Does the client feel respected and valued within the healthcare environment?
- Self-actualization – a process or action of reaching one’s full potential and self-fulfillment.
- What is important to the client in terms of what they want to achieve in life in general? What are the client’s goals that they may have for themselves in their own health and healing journey? Does the client feel satisfied, confident, and accomplished?
You can use Maslow’s Hierarchy of Needs as a guide, but it is important to be aware of the critiques and possible limitations in its application. See Video 6.1 of a conversation between Dr. Lisa Seto Nielsen and Mahidhar Pemasani.
Video 6.1: A discussion about Maslow’s Hierarchy of Needs
Criticisms of Maslow’s hierarchy are related to it being ethnocentric, based on individualistic societies, and not necessarily taking into account diversity in culture, gender, and age (Bouzenita & Wood Boulanouar, 2016; Francis & Kritsonsis, 2006; Gambrel & Cianci, 2003). It should not be arbitrarily applied to all healthcare encounters. Although you may initially focus on physiological needs to ensure the client is stable, the client may have different priorities that are more important to them. By drawing upon Indigenous knowledge, it is vital to recognize the role of community and advocacy in reaching self actualization at every level (Bennett & Shangreaux, 2005). This is particularly important in the context of systemic racism and oppression and the existing disparities among racialized populations including Black communities and Indigenous People.
IV. Levels of Priority of Care
Because of the importance of recognizing clinical deterioration in a client, a nurse must always be attuned to the set of physiological needs that are important to maintain life and prevent death. These priorities of care are related to the ABCs – airway, breathing, and circulation – introduced above. These priorities of care are often categorized as first, second, or third level, with the first level taking a priority (see Table 6.2).
Table 6.2: Priorities of care
|
Priority of care |
Examples |
|---|---|
|
First-level priority of care are problems/issues that reflect critical findings, clinical deterioration and/or are life-threatening – and therefore require urgent action. Urgent means that action must be taken immediately. |
A client in respiratory distress as evident by , nasal flaring, laboured breathing, , and decreasing oxygen levels or a client with such as chest pain or the absence of or decreasing pulse or blood pressure. |
|
Second-level priority of care are problems/issues that may lead to clinical deterioration and may become life-threatening without intervention – and therefore require prompt action. Prompt means that action must be taken quickly. |
A client with signs and symptoms such as: altered level of orientation, decreased level of consciousness/confusion, elevated temperature, increasing pain levels, and cold extremities. This may include a client with a head injury who can deteriorate quickly in some cases. You should assess if they experienced a loss of consciousness and have any associated symptoms with a concussion. |
|
Third-level priority of care are problems and issues that are typically focused on functional health, client education, and counselling. These should be addressed, but they are non-urgent and can wait until the client is stable. The problem/issue is not acute in nature, but intervention is required to support the client’s activities of daily living, their knowledge level, and their mental health and wellbeing |
A client who is post-operative and requires assistance with hygiene and mobility, a client who reports increasing stress levels and problems sleeping, or a client who is newly diagnosed with diabetes and requires education around nutrition and monitoring their blood glucose levels. |
With regard to levels of care, it is essential to consider what is most important to the client. You should treat the client as the expert in their own life – and also as the expert in decisions about their own healthcare, if they choose. Although a client may have plummeting blood pressure, you need to consider tailoring the intervening action to their wishes. Some clients may not wish for intervention in a life-threatening circumstance. Therefore, you always need to be open to the client’s wishes, but also consider whether they are able to weigh the consequences of their decision (i.e., are they competent to consent?).
Urgent Priorities of Care: Mental Health
In practice, mental health is typically not categorized as a first- or second-level priority of care unless the client is showing signs of clinical deterioration based on the examples noted in Table 6.3. In some situations, mental health may be positioned as a third-level priority of care, for example when a client is experiencing anxiety, depression, grief, but shows no signs of suicidal ideation. These symptoms should be addressed, but according to this framework, they are considered less urgent compared to first- and second-level priorities of care. However, sometimes, you should think differently about how mental health is a priority of care.
In some situations, mental health may take precedence. For example, a client who has attempted suicide or has just overdosed will probably have other physical symptoms as a result and therefore require urgent intervention and constant observation as per Table 6.3. However, the descriptions of the priorities of care presented in the table do not account for a client who has voiced a specific plan for suicide and has identified when and how. This client is at very high risk and requires urgent intervention regardless of what may be viewed as their physical health state or history. The description of priorities of care listed above does not account for this except as a third-level priority – but a client with suicide ideation or has voiced wanting to hurt others requires urgent action to protect their own wellbeing and others and the possibility of clinical deterioration as a result of their actions.
V. Intervention Types
As illustrated by the text box above, you will need to use your own judgement to determine how to act when a cue presents itself and how to categorize these interventions. This could involve four general types of interventions that you need to be aware of (see Table 6.3) including effective, ineffective, unrelated, and contraindicated. These types of interventions will become more clear as you begin to learn about normal, abnormal, and critical findings for various body systems, and how interventions and actions will affect these findings and the client.
Table 6.3: Types of interventions
|
Type of Intervention |
Example The client has no pulse, their chest is not rising, and they are not responsive. As a nurse you need to make a clinical judgment on how to act based on these cues. |
|---|---|
|
Effective (or indicated) interventions are actions that are adequate to produce the intended result and help the client. |
Begin CPR immediately. This is also an evidence-informed intervention because a delayed response results in poor outcomes as per the research. |
|
Ineffective interventions are actions that are not adequate to produce the intended result and therefore will not help the client. |
Provide mouth-to-mouth resuscitation; without compressions, the oxygen will not circulate. |
|
Unrelated (or non-essential) interventions are actions that will not produce an effect (positive or negative) and therefore will not help the client. |
Notify the client’s employer. |
|
Contraindicated interventions are actions that are not recommended because they have the potential to cause harm to the client. |
A contraindicated intervention is to delay resuscitation until a physician is present. |
Exercises: In-Class
1.
2. SPOTLIGHT APPLICATION: https://wtcs.pressbooks.pub/nursingmpc/chapter/2-6-spotlight-application/
Sam is a novice nurse who is reporting to work for his 0600 shift on the medical telemetry/progressive care floor. He is waiting to receive handoff report from the night shift nurse for his assigned patients. The information that he has received thus far regarding his patient assignment includes the following:
- Room 501: 64-year-old patient admitted last night with heart failure exacerbation. Patient received furosemide 80mg IV push at 2000 with 1600 mL urine output. He is receiving oxygen via nasal cannula at 2L/minute. According to the night shift aide, he has been resting comfortably overnight.
- Room 507: 74-year-old patient admitted yesterday for possible cardioversion due to new onset of atrial fibrillation with rapid ventricular response. Is scheduled for transesophageal echocardiogram and possible cardioversion at 1000.
- Room 512: 82-year-old patient who is scheduled for coronary artery bypass graft (CABG) surgery today at 0700 and is receiving an insulin infusion.
- Room 536: 72-year-old patient who had a negative heart catheterization yesterday but experienced a groin bleed; plans for discharge this morning.
Based on the limited information Sam has thus far, he begins to prioritize his activities for the morning. With what is known thus far regarding his patient assignment, whom might Sam plan to see first and why? What principles of prioritization might be applied?
Clinical Judgment Review: Think, Pair, Share
Read the case scenario and complete the activity below.
Case Scenario
Client admitted to orthopedic unit following an open reduction internal fixation of right lower tibia and fibula. Client was brought to the emergency department by family after falling on the stairs at home. Client reports pain currently 4 out of 10 and tolerable. Right lower leg in cast, elevated on pillows. Toes warm, capillary refill < 3 seconds, client denies numbness or tingling. Client reminded of non-weight bearing status on the right leg. Reviewed prescriptions and expectations for hospital stay. Client asks, “Why do I need insulin? I don’t have diabetes. The last time I saw my doctor, I was just told to eat less sweets and try to walk more often.”
| Lab | Normal | Yesterday | Today |
| Red Blood Cells (RBC) | 4.2 – 5.9 cells/L | 5.85 cells/L | 4.1 cells/L |
| Hemoglobin (Hgb) | 12 – 17 g/dL | 13.9 g/dL | 11 g/dL |
| Hematocrit (Hct) | 36 – 51 % | 48% | 33% |
| White Blood Cells (WBC) | 4,000 – 10,000 μL | 13,500 μL | 11,500 μL |
| Glucose | 70 – 100 mg/dL | 210 mg/dL | 280 mg/dL |
| Potassium | 3.5 – 5.0 mEq/L | 3.8 mEq/L | 3.2 mEq/L |
| Sodium | 135 – 145 mmol/L | 130 mmol/L | 134 mmol/L |
Instructions:
Pair with another student and complete the following activity on a 3×5 card.
Share your answers with the class.
Lab values are numbers (example: 2.5, 80, etc.)
- List three lab values that indicates your patient’s condition is improving
- List three lab values that indicates your patient’s condition is worsening
- List a priority nursing intervention based on one of these lab values
VI. Reflections
Remember
Prepare for the librarian visit.
- Have few EBP articles ready to discuss with the librarian
- Choose an EBP article for the EBP assignment
Key Takeaways
Type your key takeaways here.
- First
- Second
Assignment: Review Blackboard for details
- MC Library Tutorial APA Format and Quiz (90%) 2.5 points.
- Library Tutorial- Academic Integrity & Avoiding Plagiarism Quiz (90%) 2.5 points.
VII. Recommended Resources
CLINICAL JUDGMENT MEASUREMENT MODEL:https://www.nclex.com/clinical-judgment-measurement-model.page
Getting Ready for the Next-Generation NCLEX® (NGN): How to Shift from the Nursing Process to Clinical Judgment in Nursing:https://evolve.elsevier.com/education/expertise/next-generation-nclex/ngn-transitioning-from-the-nursing-process-to-clinical-judgment/
References and Attributes
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221.
- Dickison, P., Haerling, K., & Lasater, K. (2019). Integrating the National Council of State Boards of Nursing Clinical Judgment Model into nursing educational frameworks. Journal of Nursing Education, 58(2), 72-78. https://doi.org/10.3928/01484834-20190122-03
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221.
- NCSBN (2020, Spring). Next Generation NCLEX news. https://www.ncsbn.org/NGN_Spring20_Eng_02.pdf
- Padilla, R., & Mayo, A. (2017). Clinical deterioration: A concept analysis. Journal of Clinical Nursing, 27, 1360-1368. https://doi.org/10.1111/jocn.14238
- Tanner, C. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204-211. https://doi.org/10.3928/01484834-20060601-04
- Maslow, A. (1943). A theory of human motivation. Psychological Review, 50(4), 370-396. https://doi.org/10.1037/h0054346
- Bennett, M., & Shangreaux, C. (2005). Applying Maslow’s Hierarchy Theory. First Peoples Child & Family Review: a Journal of Innovation and Best Practices in Aboriginal Child Welfare Administration, Research, Policy & Practice, 2(1)89-116. https://doi.org/10.7202/1069540ar
- Bouzenita, A. I. & Wood Boulanouar, A. (2016). Maslow’s hierarchy of needs: An Islamic critique. Intellectual Discourse, 24(1), 59-81.
- Francis, N.H. & Kritsonis, W.A. (2006). A brief analysis of Abraham Maslow’s original writing of self-actualizing people: A study of psychological health. Doctoral Forum: National Journal of Publishing and Mentoring Doctoral Student Research, 3(1), 1-7.
- Critical Thinking and Clinical Reasoning: https://med.libretexts.org/Bookshelves/Nursing/Nursing_Management_and_Professional_Concepts_(OpenRN)/02%3A_Prioritization/2.04%3A_Critical_Thinking_and_Clinical_Reasoning

