Clinical Judgment Part B: Evidence-Based Nursing
Learning Objectives
At the end of this chapter, the learner will:
- Discuss ethical and legal accountability for patients’ well-being
- Apply the elements of evidence -based practice in patient clinical scenarios
Overview of this chapter
In this chapter, first, you will find the legal and ethical considerations in nursing practice. This chapter will provide the information about code of ethics, nursing practice act, social media guideline and HIPPA guidelines. The second part includes evidence-based practice. You will learn about EBP, what is it, how it is applied in nursing, steps of EBP and application in clinical scenarios.
Introduction
Nurses are responsible for being aware of the laws and regulations affecting their nursing care in the state(s) in which they are practicing. If allegations are made regarding a nurse’s professional conduct or provision of client care, the excuse “I did not know” does not hold up in a court of law or with a state’s Board of Nursing. This chapter will provide foundational legal and ethical knowledge for nursing practice in complex health care environments.
Evidence -based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.”
This chapter includes EBP definition, importance of providing EBP care to patients and its application in patient clinical scenarios.
- Legal Considerations
As discussed earlier in this guide, nurses can be reprimanded or have their licenses revoked for not appropriately following the Nurse Practice Act in the state they are practicing. Nurses can also be held legally liable for negligence, malpractice, or breach of patient confidentiality when providing patient care.
A. Negligence and Malpractice
Negligence is a “general term that denotes conduct lacking in due care, carelessness, and a deviation from the standard of care that a reasonable person would use in a particular set of circumstances.”
Malpractice is a more specific term that looks at a standard of care, as well as the professional status of the caregiver.”
To prove negligence or malpractice, the following elements must be established in a court of law:
- Duty owed the patient
- Breach of duty owed the patient
- Foreseeability
- Causation
- Injury
- Damages
To avoid being sued for negligence or malpractice, it is essential for nurses and nursing students to follow the scope and standards of practice care set forth by their state’s Nurse Practice Act; the American Nurses Association; and employer policies, procedures, and protocols to avoid the risk of losing their nursing license. Examples of nurses breach of duty that can be viewed as negligence include:
- Failure to Assess: Nurses should assess for all potential nursing problems/diagnoses, not just those directly affected by the medical disease. For example, all patients should be assessed for fall risk and appropriate fall precautions implemented.
- Insufficient monitoring: Some conditions require frequent monitoring by the nurse, such as risk for falls, suicide risk, confusion, and self-injury.
- Failure to Communicate:
- Lack of documentation: A basic rule of thumb in a court of law is that if an assessment or action was not documented, it is considered not done. Nurses must document all assessments and interventions, in addition to the specific type of patient documentation called a nursing care plan.
- Lack of provider notification: Changes in patient condition should be urgently communicated to the health care provider based on patient status. Documentation of provider notification should include the date, time, and person notified and follow-up actions taken by the nurse.
- Failure to Follow Protocols: Agencies and states have rules for reporting certain behaviors or concerns. For example, a nurse is required to report suspicion of patient, child, or elder abuse based on data gathered during an assessment.
B. Patient Confidentiality
In addition to negligence and malpractice, patient confidentiality is a major legal consideration for nurses and nursing students.
Patient Confidentiality is the right of an individual to have personal, identifiable medical information, referred to as protected health information (PHI), kept private. This right is protected by federal regulations called the Health Insurance Portability and Accountability Act (HIPAA). HIPAA was enacted in 1996 and was prompted by the need to ensure privacy and protection of personal health records and data in an environment of electronic medical records and third-party insurance payers.
There are two main sections of HIPAA law, the Privacy Rule and the Security Rule. The Privacy Rule addresses the use and disclosure of individuals’ health information. The Security Rule sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. HIPAA regulations extend beyond medical records and apply to patient information shared with others. Therefore, all types of patient information should only be shared with health care team members who are actively providing care to them.
How do HIPAA regulations affect you as a student nurse? You are required to adhere to HIPAA guidelines from the moment you begin to provide patient care. Nursing students may be disciplined or expelled by their nursing program for violating HIPAA. Nurses who violate HIPAA rules may be fired from their jobs or face lawsuits. See the following box for common types of HIPAA violations and ways to avoid them.
Common HIPAA Violations and Ways to Avoid Them
- Gossiping in the hallways or otherwise talking about patients where other people can hear you. It is understandable that you will be excited about what is happening when you begin working with patients and your desire to discuss interesting things that occur. As a student, you will be able to discuss patient care in a confidential manner behind closed doors with your instructor. However, as a health care professional, do not talk about patients in the hallways, elevator, breakroom, or with others who are not directly involved with that patient’s care because it is too easy for others to overhear what you are saying.
- Mishandling medical records or leaving medical records unsecured. You can breach HIPAA rules by leaving your computer unlocked for anyone to access or by leaving written patient charts in unsecured locations. You should never share your password with anyone else. Make sure that computers are always locked with a password when you step away from them and paper charts are closed and secured in an area where unauthorized people don’t have easy access to them. NEVER take records from a facility or include a patient’s name on paperwork that leaves the facility.
- Illegally or unauthorized accessing of patient files. If someone you know, like a neighbor, coworker, or family member is admitted to the unit you are working on, do not access their medical record unless you are directly caring for them. Facilities have the capability of tracing everything you access within the electronic medical record and holding you accountable. This rule holds true for employees who previously cared for a patient as a student; once your shift is over as a student, you should no longer access that patient’s medical records.
- Sharing information with unauthorized people. Anytime you share medical information with anyone but the patient themselves, you must have written permission to do so. For instance, if a husband comes to you and wants to know his spouse’s lab results, you must have permission from his spouse before you can share that information with him. Just confirming or denying that a patient has been admitted to a unit or agency can be considered a breach of confidentiality.
- Information can generally be shared with the parents of children until they turn 18, although there are exceptions to this rule if the minor child seeks birth control, an abortion, or becomes pregnant. After a child turns 18, information can no longer be shared with the parent unless written permission is provided, even if the minor is living at home and/or the parents are paying for their insurance or health care. As a general rule, any time you are asked for patient information, check first to see if the patient has granted permission.
- Texting or e-mailing patient information on an unencrypted device. Only use properly encrypted devices that have been approved by your health care facility for e-mailing or faxing protected patient information. Also, ensure that the information is being sent to the correct person, address, or phone number.
- Sharing information on social media. Never post anything on social media that has anything to do with your patients, the facility where you are working or have clinical, or even how your day went at the agency. Nurses and other professionals have been fired for violating HIPAA rules on social media.
Activity
- View the Social Media Guidelines for Nurses video from the National Council of State Boards of Nursing (NCSBN) on using social media responsibly.
- Discuss how this impacts your role as a nurse to protect your patient’s privacy
- Share a recent example from the news about the inappropriate use of social media that impacted on an individual and its negative impacts.
C. Social Media Guidelines
Nursing students, nurses, and other health care team members must use extreme caution when posting to Facebook, Instagram, Twitter, Snapchat, and other social media sites. Information related to patients, patient care, and/or health care agencies should never be posted on social media; health care team members who violate this guideline can lose their jobs and may face legal action and students can be disciplined or expelled from their nursing program. Be aware that even if you think you are posting in a private group, the information can become public.
The American Nurses Association (ANA) has established the following principles for nurses using social media
- Nurses must not transmit or place online individually identifiable patient information.
- Nurses must observe ethically prescribed professional patient-nurse boundaries.
- Nurses should understand that patients, colleagues, organizations, and employers may view postings.
- Nurses should take advantage of privacy settings and seek to separate personal and professional information online.
- Nurses should bring content that could harm a patient’s privacy, rights, or welfare to the attention of appropriate authorities.
- Nurses should participate in developing organizational policies governing online conduct.
In addition to these principles, the ANA has also provided these tips for nurses and nursing students using social media:
- Remember that standards of professionalism are the same online as in any other circumstance.
- Do not share or post information or photos gained through the nurse-patient relationship.
- Maintain professional boundaries in the use of electronic media. Online contact with patients blurs this boundary.
- Do not make disparaging remarks about patients, employers, or coworkers, even if they are not identified.
- Do not take photos or videos of patients on personal devices, including cell phones.
- Promptly report a breach of confidentiality or privacy.
Read more about the ANA’s Social Media Principles.
Exercises
D. Code of Ethics
In addition to legal considerations, there are also several ethical guidelines for nursing care.
There is a difference between morality, ethical principles, and a Code of Ethics. Morality refers to “personal values, character, or conduct of individuals within communities and societies. A n ethical principle is a general guide, basic truth, or assumption that can be used with clinical judgment to determine a course of action.
Four common ethical principles are
- beneficence (do good)
- nonmaleficence (do no harm)
- autonomy (control by the individual)
- and justice (fairness).
A code of ethics is set for a profession and makes their primary obligations, values, and ideals explicit.
The American Nursing Association (ANA) guides nursing practice with the Code of Ethics for Nurses. This code provides a framework for ethical nursing care and a guide for decision-making. The Code of Ethics for Nurses serves the following purposes:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.
The ANA Code of Ethics contains nine provisions. See a brief description of each provision in the following box.
Provisions of the ANA Code of Ethics
The nine provisions of the ANA Code of Ethics are briefly described below. The full code is available to read for free at Nursingworld.org.
Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
Provision 8: The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
The ANA Center for Ethics and Human Rights
In addition to publishing the Code of Ethics, the ANA Center for Ethics and Human Rights was established to help nurses navigate ethical and value conflicts and life-and-death decisions, many of which are common to everyday practice.
II. Evidence-Based Practice in Nursing
A. What is Evidence-Based Practice?
Evidence-based practice is defined as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the healthcare consumer’s history and condition, as well as health care resources; and patient, family, group, community, and population preferences and values.”
Utilizing evidence-based practice means that nurses and nursing students provide patient care based on research studies and clinical expertise and do not just do something “because that’s the way we’ve always done it.” A simple example of nurses promoting evidence-based practice to help patients is using peppermint to relieve nausea. Throughout history, peppermint was used for an upset stomach and to relieve the feeling of nausea. This idea was frequently rejected in the medical field because there was no scientific evidence to support it. However, In 2016, Lynn Bayne and Helen Hawrylack, two nurse researchers, developed a peppermint inhaler for patients to use when they were feeling nauseated and found it was 93% effective in relieving nausea.
Nursing students should implement evidence-based practice as they begin their nursing career by ensuring the resources they use to prepare for patient care are valid and credible.

B. Why is EBP Important?
Evidence-based practice looks at clinical expertise, research evidence, and patients’ needs and values.

Clinical Expertise
- Clinical Expertise is the provider’s judgment about what works best in similar patients or in similar situations.
- Health is complex and there isn’t high-quality research on every topic.
- Through years of practice, healthcare providers develop clinical expertise that guides patient care decisions.
- This clinical judgment is essential for applying evidence-based practice.
Best Scientific Evidence
- The best scientific evidence is the results of the best available scientific studies. It is used to find out which treatments, diagnostic methods, or ways of predicting a patient outcome work best.
- Scientists carefully design studies to measure how well things such as treatment and diagnostic tests work.
- Scientific evidence can provide a higher-level view than expert opinions or objective data to help inform healthcare decisions, and is one of the important pieces of evidence-based practice.
Patient’s Needs and Values
- Patients’ or clients’ needs and values are what is important for the patient or client and what healthcare options best match those values.
- There are many conditions where patient needs and preferences are important factors in choosing the right treatment or screening option.
- Cost of care, quality of life, and personal beliefs are all important considerations.
- Patients should be partners in their care and help decide what type of healthcare is best for them.
- Evidence-based practice recognizes that patient values are essential in determining care.
C. The Five Steps of EBP
Now that we have identified why evidence-based practice is important, let’s address the steps of evidence-based practice. There are five steps of evidence-based practice that provide a framework for approaching a question, also known as the Five A’s:
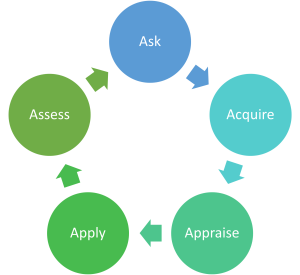
- Step 1: Ask a well-built question
- Step 2: Acquire evidence
- Step 3: Appraise the evidence
- Step 4: Apply the evidence along with clinical judgment and patient values
- Step 5: Assess the results
Activity
Examples
Remember
Prepare for the librarian visit.
- Have few EBP articles ready to discuss with the librarian
- Choose an EBP article for the EBP assignment
Key Takeaways
Type your key takeaways here.
- First
- Second
Assignment: Review Blackboard for details
- MC Library Tutorial APA Format and Quiz (90%) 2.5 points.
- Library Tutorial- Academic Integrity & Avoiding Plagiarism Quiz (90%) 2.5 points.
III. Application in Practice
Nursing Case Study
 Your patient is a 48-year-old premenopausal, multiparous female suffering from urinary stress incontinence. She has been doing pelvic floor exercises on her own, following instructions on a patient education handout she got from her doctor, to improve the symptoms, but she is not happy with the results and isn’t sure if she is doing the exercises correctly. She is very upset and embarrassed by her incontinence, but does not want to consider surgery because of the side effects she has heard about, the cost of the surgery and the idea of being under anesthesia. She read about pelvic floor biofeedback on the Internet and wonders if that would be another thing she could try in addition to her exercises to help improve her pelvic floor training. She feels very hindered by the problem and wants her life back.
Your patient is a 48-year-old premenopausal, multiparous female suffering from urinary stress incontinence. She has been doing pelvic floor exercises on her own, following instructions on a patient education handout she got from her doctor, to improve the symptoms, but she is not happy with the results and isn’t sure if she is doing the exercises correctly. She is very upset and embarrassed by her incontinence, but does not want to consider surgery because of the side effects she has heard about, the cost of the surgery and the idea of being under anesthesia. She read about pelvic floor biofeedback on the Internet and wonders if that would be another thing she could try in addition to her exercises to help improve her pelvic floor training. She feels very hindered by the problem and wants her life back.
Complete the following:
Exercises
Framing good questions
Describe the subject of the question.
It may be helpful to phrase the question in this form: “How would I describe a group of patients similar to this one? What are the relevant characteristics?”
Define which intervention you are considering for the specific patient or population.
It is sometimes helpful to name a second intervention with which to compare the first.
This might be another treatment, placebo, or ‘usual care.’
For example, diagnosis via a traditional X-ray is often compared to diagnosis with an MRI. However, it is not always necessary to include a comparison.
Define the type of outcome you wish to assess.
There are many possible outcomes. Try to focus on patient-oriented outcomes like death, disability or discomfort. These could include mortality, disease progression, results of a diagnosis test, confidence/anxiety, cost effectiveness and more.
Let’s take a look at our PICO examples from before.
Example 1
Patient/problem/population: mid-50s male with a 30 pack-year history of smoking
Intervention: bupropion
Comparison intervention: nicotine replacement therapy
Outcome: long-term abstinence from smoking
A well-built clinical question for these PICO elements would be: In a 55 year old man, would the administration of bupropion therapy versus nicotine replacement therapy lead to long-term abstinence from smoking?
Example 2
Patient/problem/population: woman in her 40s with no family history of breast cancer
Intervention: mammograms every three years
Comparison: yearly mammograms
Outcome: early detection of breast cancer
A well-built clinical question for these PICO elements would be: In a 42 year old woman with no family history of breast cancer, are mammograms every three years as effective in detecting breast cancer as yearly mammograms?
Here are some other examples of clinical questions. Even though we don’t have the example clinical scenario or the PICO frameworks for the below questions, you can easily tell what the most important elements of the patient scenarios are:
- In a 50 year old man with low back pain, is physical therapy as effective at relieving pain as surgery?
- In a 34 year old woman with chronic cold sores, does taking zinc work help to prevent cold sores?
IV. Reflections
Key Takeaways
Type your key takeaways here.
- First
- Second
Interactive Session
Librarian Visit (Q&A Live Sessions – 30 minutes)
Assignment: Medication Safety Assignment
Please review Blackboard for assignment instructions
V. Recommended Resources
EBP Tutorial: Module 1: Intro to EBP https://guides.mclibrary.duke.edu/ebptutorial
WHO: Medication Without Harm:https://youtu.be/MWUM7LIXDeA?si=-Dz9XoASdVnEUeuz
EBP Basics Free Online Course: https://fuld.nursing.osu.edu/ebp-basics-free-online-course
https://www.softchalkcloud.com/lesson/serve/Au0xZt1zQdV67O/html
https://guides.mclibrary.duke.edu/ebptutorial
ETHICAL DILEMMAS: https://wtcs.pressbooks.pub/nursingmpc/chapter/6-3-ethical-dilemmas/
PROTECTING YOUR NURSING LICENSE: https://wtcs.pressbooks.pub/nursingmpc/chapter/5-5-protecting-your-nursing-license/
PICO:https://youtu.be/XyPTdN3ZBss
Evidence Hierarchies for EBP:https://youtu.be/inIhKb9CY6o?si=CAxwm9G_V9FHq-G7
Introduction to Nursing research and Evidence-Based Practice(EBP) (Nursing Research 1): https://youtu.be/yYpGiEoUZPA?si=YH8uIhMY6sMknOM4
References and Attributions
- Missouri Department of Health & Senior Services. (n.d.). Negligence and malpractice. https://health.mo.gov/living/lpha/phnursing/negligence.php#:~:text=Negligence%20is%3A,a%20particular%20set%20of%20circumstances. ↵
- Vera, M. (2020). Nursing care plan (NCP): Ultimate guide and database. https://nurseslabs.com/nursing-care-plans/#:~:text=Collaborative%20interventions%20are%20actions%20that,to%20gain%20their%20professional%20viewpoint. ↵
- Patterson, A. (2018, July 3). Most common HIPAA violations with examples. Inspired eLearning. https://inspiredelearning.com/blog/hipaa-violation-examples/ ↵
- Karimi, H., & Masoudi Alavi, N. (2015). Florence Nightingale: The mother of nursing. Nursing and Midwifery Studies, 4(2), e29475. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4557413/ ↵
- American Nurses Association. (n.d.). About ANA. https://www.nursingworld.org/ana/about-ana/ ↵
- American Nurses Association. (n.d.). Scope of practice. https://www.nursingworld.org/practice-policy/scope-of-practice/ ↵
- American Nurses Association. (n.d.). Social media. https://www.nursingworld.org/social/ ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. American Nurses Association. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/coe-view-only/ ↵
- Nurses Service Organization and CAN Financial. (2020, June). Nurse professional liability exposure claim report (4th ed.). https://www.nso.com/Learning/Artifacts/Claim-Reports/Minimizing-Risk-Achieving-Excellence ↵
- “aid9688616-v4-728px-Get-a-California-Endorsement-for-Your-Nursing-License-Step-11.jpg” by unknown
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- ChristianaCare News. (2016, May 16). Nurse researchers develop peppermint inhaler to relieve post-op nausea. https://news.christianacare.org/2016/05/nurse-researchers-develop-peppermint-inhaler-to-relieve-post-op-nausea/ ↵
- Modified from https://wtcs.pressbooks.pub/nursingfundamentals/chapter/1-6-legal-considerations-and-ethics/#footnote-709-3
- Boehning, A. P., & Haddad, L. M. (2023). Nursing Practice Act. In StatPearls. StatPearls Publishing.
- Ernstmeyer, K., & Christman, E. (Eds.). (2021). Open RN Nursing Fundamentals by Chippewa Valley Technical College

