3 Rest, Comfort and Mobility: Pain and Analgesics ; Inflammation and Anti-inflammatory drugs
Effective pain and discomfort management is crucial for achieving restorative sleep, which is essential for the body to regain strength and return to a healthy state. In this chapter, you will explore various methods to alleviate your patient’s pain, enhance comfort, and promote beneficial rest and sleep.
Learning Objectives
- Explain the mechanism of action, indication for use, adverse effects, and nursing process implications for opioids, salicylates, nonnarcotic analgesics, antipyretics, and nonsteroidal anti-inflammatory analgesics.
- Contrast the use of opioid analgesics in opioid-naïve and opioid-tolerant patients.
- Describe characteristics and treatment of opioid toxicity.
I. Pain and Mobility Introduction
Complaints of pain are among the most common reasons individuals seek medical care. Pain signals indicate that something in the body is not quite right, which could potentially affect one’s quality of life. Pain assessment and treatment will become an important part of one’s daily work, whether it be a headache, a broken bone, labor pain, chest pain, or another condition.
As a nurse, you will care for patients experiencing various types of pain manifestations and responses. It will be important for you to understand the various pharmacological and non-pharmacological treatment methods available for your patients.
Concepts Related to Pain
This resource provides a basic introduction to the concept of pain as it relates to pharmacology. Pain is an unpleasant sensory and emotional experience linked to actual or potential tissue damage.
The Concept of Mobility and the Musculoskeletal System
Mobility is defined as intentional physical movement, encompassing simple gross movements, complex fine movements, and coordination; it also describes the state or ability to be mobile or moveable.
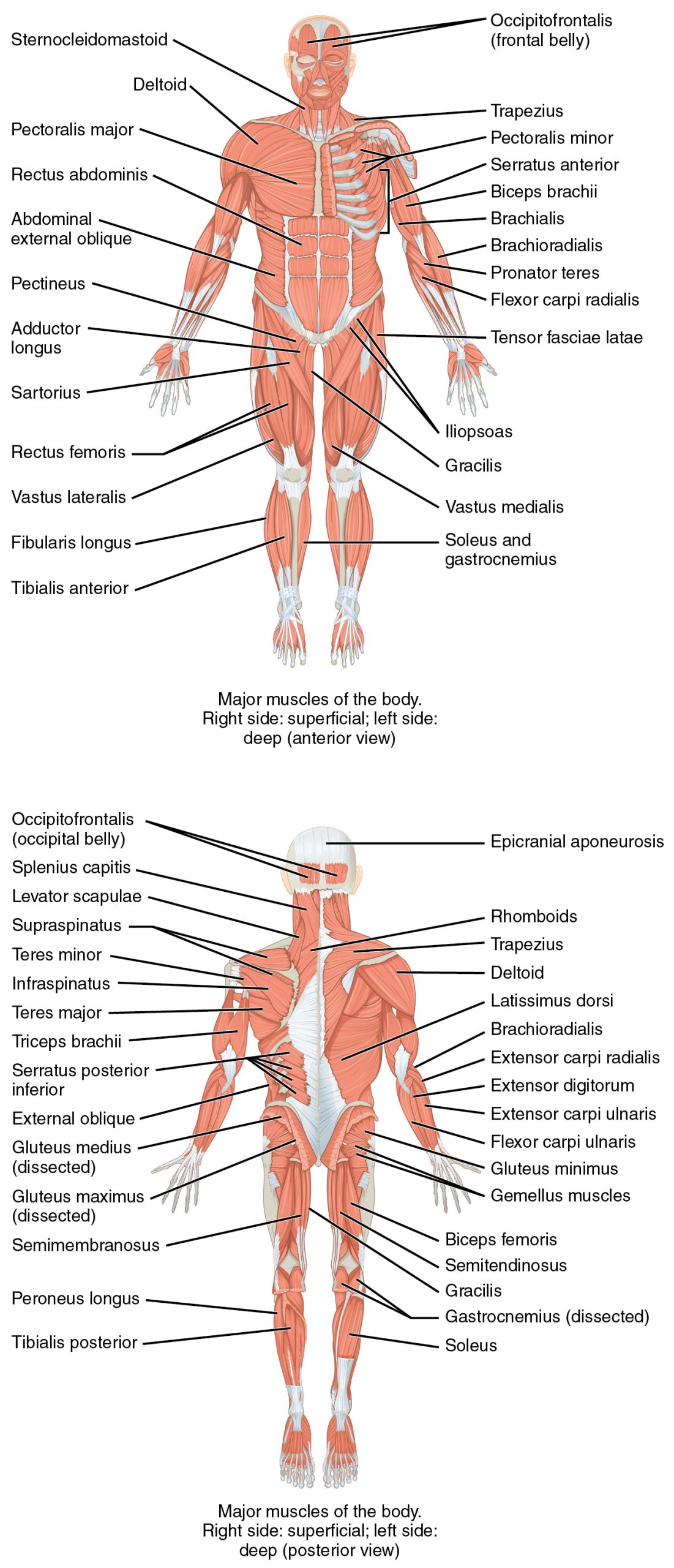
The musculoskeletal system consists of the muscular and skeletal systems, which work together to support and move the body. The bones of the skeletal system protect the body’s organs, support the body’s weight, and give the body shape. The muscles of the muscular system attach to these bones, pulling on them to allow for movement of the body. See the image below for an illustration of the musculoskeletal system.
Muscles
The body contains three types of muscle tissue: skeletal, smooth, and cardiac. See the image below for different types of muscle: (a) Skeletal muscle, (b) Smooth muscle, and (c) Cardiac muscle.
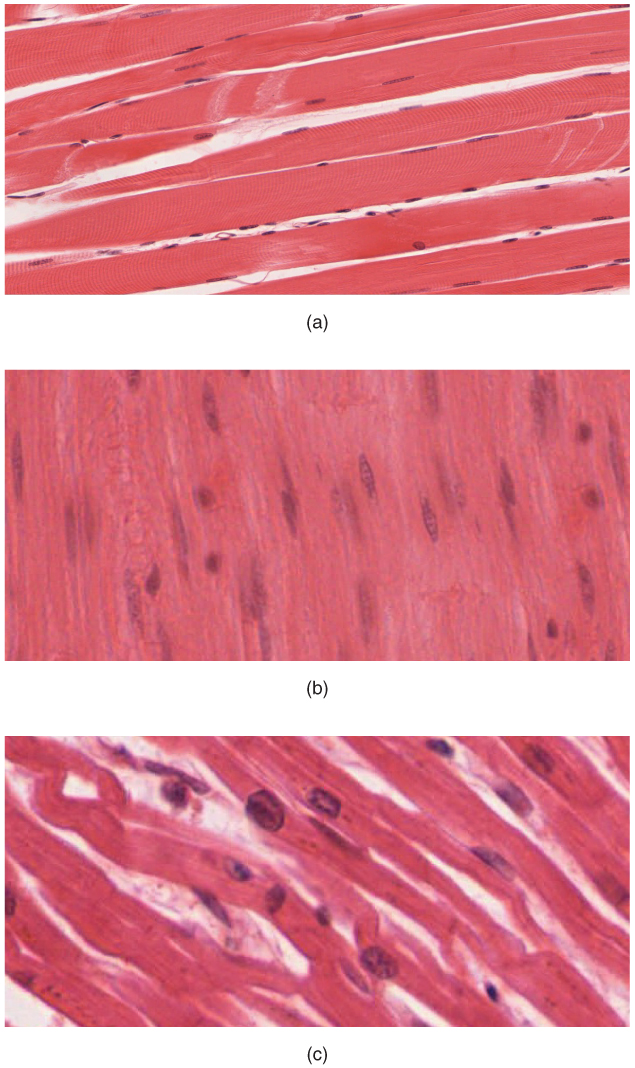
Skeletal muscle is voluntary and striated. These are the muscles that attach to bones and control conscious movement. Smooth muscle is involuntary and non-striated. It is found in the body’s hollow organs, such as the stomach, intestines, and around blood vessels. Cardiac muscle is involuntary and striated. It is found only in the heart and is specialized to help pump blood throughout the body.
When a muscle fiber receives a signal from the nervous system, myosin filaments are stimulated, pulling actin filaments closer together. This shortens sarcomeres within a fiber, causing it to contract.
Knowledge Check
You are reviewing the medical record of your assigned patient, who is an 87-year-old hospitalized due to a left femur from a fall. The patient is non-verbal and has a past medical history of hypertension, high cholesterol, and chronic back pain.
Answer the following questions using the case study above.
II. Physiology of Pain
Pain occurs when tissue damage occurs in the body. Tissue damage activates pain receptors in peripheral nerves. Nociceptors, the nerve endings that respond to painful stimuli, are located in arterial walls, joint surfaces, muscle fascia, periosteum, skin, and soft tissue. They are barely present in most internal organs.
The cause of tissue damage may be physical (e.g., heat, cold, pressure, stretch, and spasm), ischemic (loss of circulation), or chemical (pain-producing substances that are released into the extracellular fluid surrounding the nerve fibers that carry the pain signal). These pain-producing substances activate pain receptors, increase the sensitivity of pain receptors, or stimulate the release of inflammatory substances (e.g., prostaglandins).
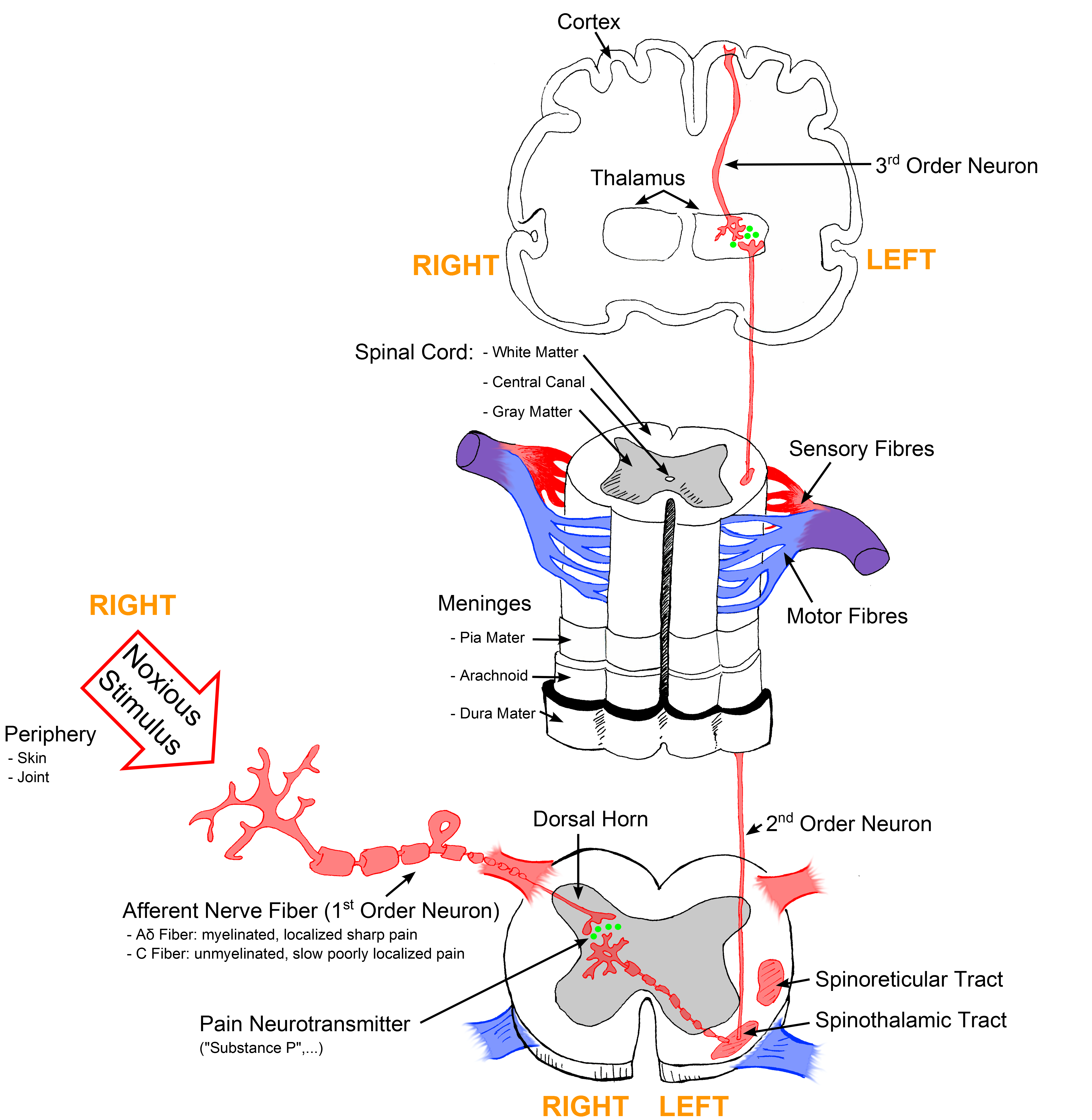
For a person to feel pain, the signal from the nociceptors in peripheral tissues must be transmitted to the spinal cord and then to the hypothalamus and cerebral cortex of the brain. The signal is transmitted to the brain by two types of nerve cells (A-delta and C fibers). The dorsal horn of the spinal cord is the relay station for information from these fibers. In the brain, the thalamus is the relay station for incoming sensory stimuli, including pain. From the thalamus, the pain messages are relayed to the cerebral cortex, where they are perceived. The image below illustrates how the pain signal is transmitted from peripheral tissues to the spinal cord and then to the brain.
Types of Pain: Acute pain
Acute pain: Acute pain usually comes on suddenly and is caused by something specific. It is sharp in quality. Acute pain usually does not last six months or longer. It goes away when there is no underlying cause for the pain. Causes of acute pain include:
- Surgery
- Broken bones
- Dental work
- Burns or cuts
- Labor and childbirth
After acute pain goes away, a person can go on with life as usual.
Chronic pain: chronic pain is pain that is ongoing and usually lasts longer than six months. This type of pain can continue even after the injury or illness that caused it has healed or gone away. Pain signals remain active in the nervous system for weeks, months, or years. Some people suffer chronic pain even when there is no past injury or apparent body damage. Chronic pain is linked to conditions including:
- Headache
- Arthritis
- Cancer
- Nerve pain
- Back pain
- Fibromyalgia pain
- Phantom pain
People who have chronic pain can experience physical effects that are stressful on the body. These include tense muscles, limited ability to move around, a lack of energy, and appetite changes. Emotional effects of chronic pain include depression, anger, anxiety, and fear of re-injury. Such a fear might limit a person’s ability to return to regular work or leisure activities.
There are more types of pain, including neuropathic pain, somatic, superficial,
visceral and cancer pain.
Interactive Activity
III. Clinical Reasoning and Decision-Making for Pain and Mobility
Let’s Think of Why. Recognizing Cues
Although there are numerous details to consider when administering medications, it is always important to consider what you give and why.
Nurses always make decisions, but making decisions requires a complex thinking process. Many valuable tools can support your thinking through clinical judgments and can be found online. This book uses the nursing process and clinical judgment language to help you understand the application of medication to your clinical practice.
Before administering any medication, nurses should assess and gather information to analyze and prioritize a hypothesis.
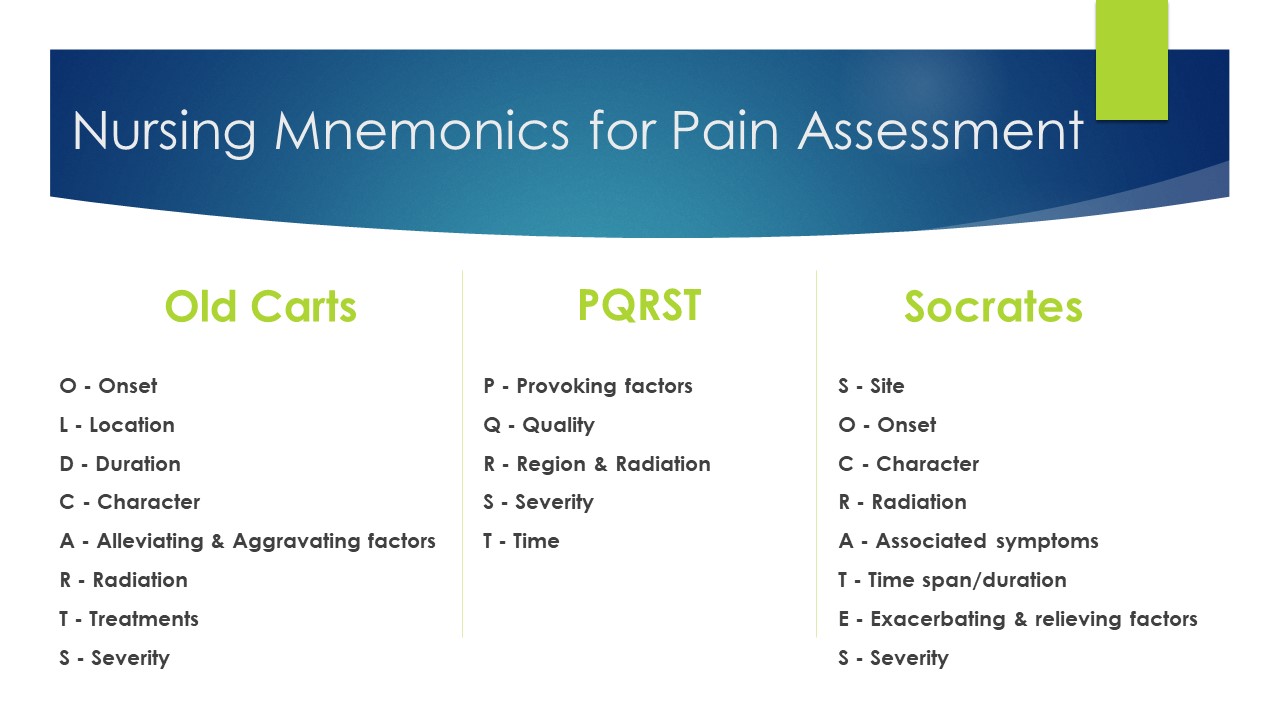
For example, when considering pain medication, a comprehensive pain assessment should be performed, including determining the pain scale and identifying an acceptable pain level for the patient. See the image below for standard nursing mnemonics for pain assessment.
Additional baseline information to collect before administering any analgesic or musculoskeletal medication includes any history of allergy or a previous adverse response.
Lifespan Considerations
Most medications are calculated based explicitly on the patient’s weight and renal function. Patient age and size are especially vital in pediatric patients. A child’s stage of development and the size of their internal organs significantly impact how the body absorbs, digests, metabolizes, and eliminates medications.
Visual pain scales have been developed as a tool of communication about pain with children through patients at the end of life. For children ages 2 months to 7 years and for adults who are non-verbal or intubated, a behavioral pain assessment scale is used to evaluate pain. This scale is known as a FLACC (Face, Legs, Activity, Cry, Consolability) is used.
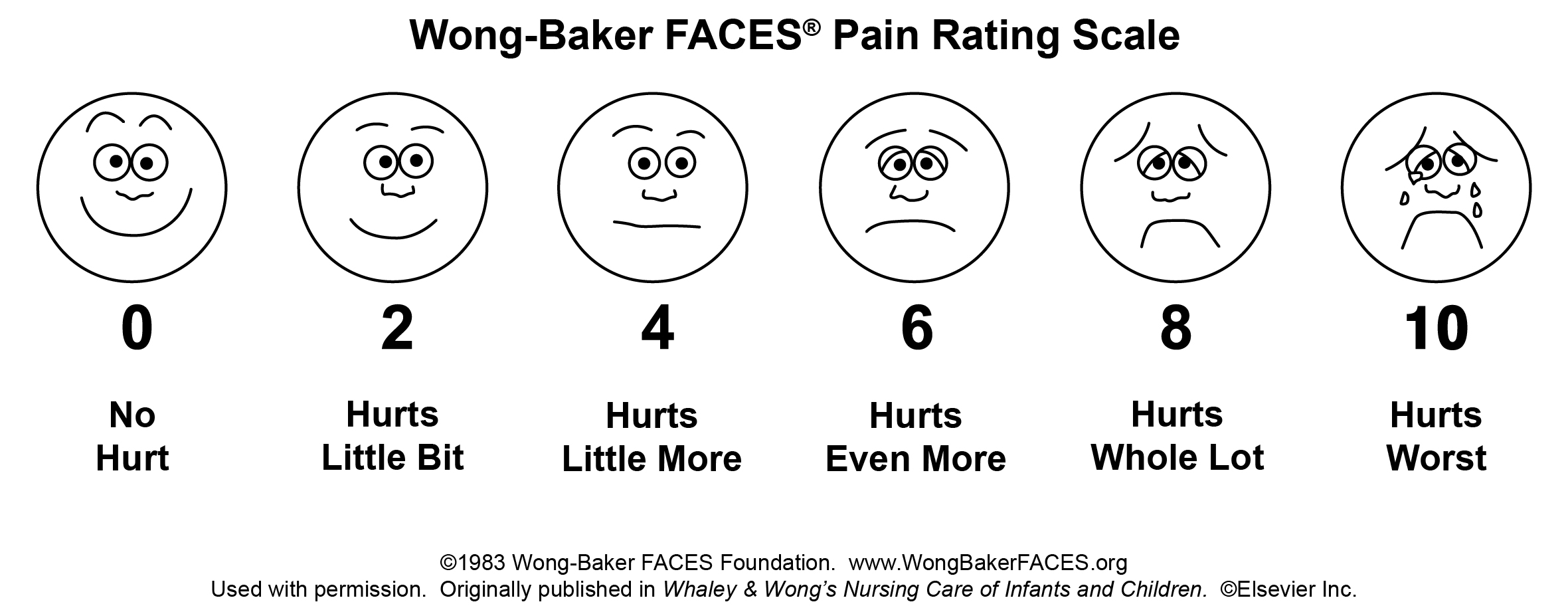
Wong-Baker FACES Pain Rating Scale
To use the face pain scale, use the following evidence-based instructions.
- Explain to the patient that each face represents a person with no pain (hurt), some, or a lot of pain.
- Explain, “Face 0 doesn’t hurt at all. Face 2 hurts just a little. Face 4 hurts a little more. Face 6 hurts even more. Face 8 hurts a whole lot. Face 10 hurts as much as you can imagine, although you don’t have to be crying to have this worst pain.”
- Ask the patient to choose the face that best represents their pain.
Knowledge Check

When you enter the patient’s room, you observe the patient is restless and crying. The patient’s spouse is at the bedside and expresses concern about their partner’s lack of sleep throughout the night.
Interventions
Analgesics used to treat pain are categorized as non-opioid, opioid, and adjuvant medications. The following sections will introduce different classes of analgesics and musculoskeletal medications with specific administration considerations, therapeutic effects, adverse/side effects, and teaching needed for each class of drugs. These medications are available in many forms, such as oral tablets, oral liquids, injections, inhalation, and transdermal. Some products contain more than one medicine (for example, oxycodone and acetaminophen) to enhance pain relief.
Non-Opioid Analgesics
Non-opioid analgesics include acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin which is considered to be a salicylate NSAID.
Acetaminophen: The Mechanism of Action of Acetaminophen is still somewhat unknown. However, it inhibits the synthesis of prostaglandins that may mediate pain and fever, primarily in the CNS. Acetaminophen is not an anti-inflammatory agent.
Indications for Use: Acetaminophen is used to treat mild pain and reduce fever. It is indicated for headaches, minor arthritis-related pain, and muscular aches, but does not have anti-inflammatory properties.
Nursing Considerations Across the Lifespan: Acetaminophen is safe for all ages and can be administered using various routes. However, due to the risk of hepatotoxicity, special dosing considerations are required for pediatric patients and older adults and caution is taken for patient with hepatic/renal disease, and alcohol use disorders.
Older adults are more susceptible to the harmful effects of medications. Caution should be used with administration. The suggested maximum safe dose for everyone should not exceed 4000 mg (4 g) in 24 hours to avoid hepatic damage. Persons with alcohol use disorders should also have lower doses due to the risk of hepatotoxicity.
If an overdose occurs, the antidote is acetylcysteine and the dosage for the antidote is dependent on the serum acetaminophen level.
Patient Teaching and Education
Medications should be taken as directed, and the dosing schedule should be followed appropriately. Caution: patients should not take multiple medications that have acetaminophen at the same time. Patients should not take the medication for more than ten days. Additionally, patients should avoid using alcohol while taking these medications. Severe liver damage may occur if a patient consumes three or more alcoholic drinks every day while using this product. If a rash occurs, this should be reported to the healthcare provider, and the medication should be promptly stopped. The use of drugs may interfere with blood glucose monitoring. If a fever lasts over three days or exceeds 39.5 C, this should be reported to the healthcare provider.
Non-steroidal Anti-inflammatories (NSAIDs)
Non-steroidal anti-inflammatories have analgesic, antipyretic, and anti-inflammatory properties. Examples of these medications includes a Propionic acid derivative NSAID such as ibuprofen and a salicylate derivative medication such as aspirin which is also known as acetylsalicylic acid (ASA).
ASA also has antiplatelet effects. ASA and other NSAIDs relieve pain by inhibiting the biosynthesis of prostaglandin by different forms of the COX enzyme. COX2 inhibitors are selective and only inhibit the COX-2 enzyme. As a result of the inhibition of COX1 by an NSAID, there is decreased protection of the stomach lining, and gastric irritation and bleeding may occur.
Acetylsalicylic Acid Mechanism of Action: Acetylsalicylic acid (aspirin) is a non-opioid NSAID analgesic, and anti-pyretic. It reduces inflammation and fever by inhibiting the production of prostaglandins. ASA also decreases platelet aggregation.
Indications for Use: Aspirin treats mild to moderate pain, fever, and inflammatory conditions. Once-daily dosages are also used to reduce the risk of heart attack and stroke. Nursing Considerations Across the Lifespan: ASA is safe for most adults and children older than 12 years of age. However, it is not the first choice of anti-inflammatory for children and should not be used with children at risk for Reye’s syndrome. ASA is not considered safe for pregnant or nursing women.
Adverse/Side Effects: ASA may cause toxicity, intolerance, or hypersensitivity. If an overdose occurs, emergency gastric procedures may be needed, such as gastric lavage. Adverse effects of ASA include GI upset, GI bleeding, and tinnitus (ringing of the ears). ASA may cause a severe allergic reaction, which may include:
- hives
- Angioedema (swelling underneath the skin such as the face, lips, tongue, eyelids)
- shock
- difficulty breathing
Stomach bleeding warning: this product contains an NSAID, which may cause severe stomach bleeding. The chance for bleeding is higher if a patient:
- takes a higher dose or takes it for a longer time than directed
- takes other drugs containing prescription or nonprescription NSAIDs (aspirin, ibuprofen, naproxen, or others)
- has had stomach ulcers or bleeding problems
- takes a blood-thinning (anticoagulant) or steroid drug
- is age 60 or older
- has 3 or more alcoholic drinks every day while using this product
ASA is contraindicated if the patient has a bleeding disorder such as hemophilia or a recent history of bleeding in the stomach or intestine.
Patient Teaching & Education: Patients should avoid concurrent use of alcohol while taking medication to prevent gastric irritation. This medication should be out of the reach of children. Patients should also report tinnitus, unusual bleeding, or fever lasting over 3 days to the healthcare provider. s should also pause using ASA if going for surgery within one week. However, if on ASA for anti-platelet properties, patients should have alternative measures for preventing MI and stroke.
Ibuprofen
Propionic Acid Derivatives Mechanism of Action: Prevents prostaglandin synthesis by inhibiting cyclooxygenase, and reduces fever.
Indications for Use: pain reliever, anti-inflammatory effects that is helpful for decreasing inflammation for rheumatoid and osteoarthritis and dysmenorrhea symptoms.
Adverse/Side Effects: dyspepsia, gastritis, nausea/vomiting, GI bleeding, hypersensitivity, tinnitus, Steven-Johnson’s syndrome and decrease in RBC’s, WBC’s and platelets.
Patient Teaching & Education: Advise patients to not take other medications such as aspirin with other NSAIDs such as ibuprofen, it can lead to GI upsets and/or GI bleeding. Patients should avoid drinking alcohol while taking this medication, GI distress or ulcers in the GI system can result. NSAIDs should be taken with meals or a snack to decrease GI upset. Prolong bleeding time can occur with NSAIDs therefore, patients should observe for bleeding gums, stool that is black or tarry in color, petechiae or ecchymoses.
Opioid Analgesics
Opioid analgesics are prescribed for moderate to severe pain. They are delivered through a variety of routes.
Morphine sulfate is a prototype that is at the top of the WHO ladder and is used to treat severe pain. It is also commonly used to treat cancer pain and for pain at the end of life because there is no “ceiling effect,” meaning the higher the dose, the higher the level of analgesia. We will use morphine as an example of an opioid drug.
Mechanism of Action: Morphine binds to opioid receptors in the CNS and alters the perception of and response to painful stimuli while producing generalized CNS depression.
Indications for Use: Morphine is indicated for the relief of moderate to severe acute and chronic pain and for pulmonary edema.
Nursing Considerations Across the Lifespan: Morphine is safe for all ages. However, it should be used cautiously in patients with liver and renal impairment.
Adverse/Side Effects: Adverse effects include respiratory depression, hypotension, light-headedness, dizziness, sedation, constipation, nausea, vomiting, and diaphoresis, psychological dependence, urinary retention.
Patient Teaching & Education: Patients should be advised regarding the risks associated with opioid analgesic use. Please see the outlined “Special Considerations” for usage below.
Respiratory Depression: Respiratory depression is the primary risk of morphine sulfate. Respiratory depression occurs more frequently in elderly or debilitated patients and in those suffering from conditions accompanied by hypoxia, hypercapnia, or upper airway obstruction, for whom even moderate therapeutic doses may significantly decrease pulmonary ventilation.
Use morphine with extreme caution in patients with chronic obstructive pulmonary disease or cor pulmonale and in patients having a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression. In such patients, even usual therapeutic doses of morphine sulfate may increase airway resistance and decrease respiratory drive to the point of apnea. Consider alternative non-opioid analgesics, and use morphine sulfate only under careful medical supervision at the lowest effective dose in such patients.
Misuse, Abuse, and Diversion of Opioids: Morphine sulfate is an opioid agonist and a Schedule II controlled substance. People with addiction disorders seek such drugs. Diversion of Schedule II products is an act subject to criminal penalty. Morphine can be abused like other opioid agonists, legal or illicit. This should be considered when prescribing or dispensing morphine sulfate in situations where there is an increased risk of misuse, abuse, or diversion. Morphine may be abused by crushing, chewing, snorting, or injecting the product. These practices pose a significant risk to the abuser that could result in overdose and death.
Interactions with Alcohol and Drugs of Abuse: Morphine has addictive and potentially fatal effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression because respiratory depression, hypotension, profound sedation, coma, or death may result.
Opioid Antagonists
Naloxone is an opioid antagonist.
Mechanism of Action: Naloxone reverses analgesia and the CNS and respiratory depression caused by opioid agonists. It competes with opioid receptor sites in the brain and, thereby, prevents binding with receptors or displaces opioids already occupying receptor sites.
Indications for Use: Naloxone is indicated for the complete or partial reversal of opioid depression, including respiratory depression induced by natural and synthetic opioids.
Adverse/Side Effects: Adverse effects include tremors, drowsiness, sweating, respiratory depression, hyper/hypotension, nausea, and vomiting, and confusion. Patients may also experience acute narcotic abstinence syndrome. Additionally, if naloxone reverses an opioid that was indicated for pain, the pain may return.
Patient Teaching & Education
Patients should be advised regarding the risks associated with opioid analgesic use. Patients and their families should be provided information about how to use opioid antagonists from pharmacists. Patients may also be provided with a naloxone kit.
Special Considerations
Postoperative: The following adverse events have been associated with the use of naloxone hydrochloride injection in postoperative patients: hypotension, hypertension, ventricular tachycardia and fibrillation, dyspnea, pulmonary edema, and cardiac arrest. Death, coma, and encephalopathy have been reported as results of these events. Excessive doses of naloxone in postoperative patients may result in a significant reversal of analgesia and may cause agitation.
Opioid Reversal: Abrupt reversal of opioid depression may result in nausea, vomiting, sweating, tachycardia, increased blood pressure, tremulousness, seizures, ventricular tachycardia and fibrillation, pulmonary edema, and cardiac arrest, which may result in death.
Opioid Dependence: The inability to function normally in the absence of the drug. Opioid dependency can be both psychological and physical. The moment that the drug is discontinued or there is an abrupt reversal of opioid effects in persons who are experiencing dependency on opioids, it may precipitate an acute withdrawal syndrome, which may include, but is not limited to, the following signs and symptoms: anxiety, body aches, fever, sweating, runny nose, sneezing, piloerection, yawning, weakness, shivering or trembling, nervousness, restlessness or irritability, diarrhea, nausea or vomiting, abdominal cramps, increased blood pressure, and tachycardia. In the neonate, opioid withdrawal may also include convulsions, excessive crying, and hyperactive reflexes.
Interactive Activity
Knowledge Check
After performing your pain assessment, you administer morphine 4mg orally per the physical order.
Media Attributions
- Anterior_and_Posterior_Views_of_Muscles © OpenStax
- Skeletal_Smooth_Cardiac © OpenStax College is licensed under a CC BY (Attribution) license
- Sketch_colored_final © Bettina Guebeli is licensed under a CC BY (Attribution) license
- Wong-Baker Faces Pain Rating Scale
- Image 1

