7 Perfusion: Hypertension and Antihypertensives, Hyperlipidemia and Antihyperlipidemic
In the intricate system of cardiovascular health, the relationship between perfusion, hypertension, and dyslipidemia is deeply intertwined, each influencing the others in complex ways. Perfusion, the process of delivering oxygenated blood to tissues throughout the body, is critically dependent on maintaining optimal blood pressure and lipid levels. Hypertension, or elevated blood pressure, disrupts this balance, leading to increased strain on the heart and blood vessels, which can ultimately impair perfusion and contribute to the development of cardiovascular diseases. Similarly, dyslipidemia, characterized by abnormal levels of lipids in the blood, exacerbates this risk by promoting atherosclerosis. In this condition, fatty deposits build up in the arteries, further impeding blood flow and elevating blood pressure.
This chapter will explore the intricate connections between these conditions, beginning with understanding the etiology, pathophysiology, and clinical manifestations of blood pressure control. We will discuss non-pharmacological measures to manage hypertension, emphasizing lifestyle modifications that can profoundly impact reducing cardiovascular risk. The chapter will then delve into the pharmacological management of hypertension, providing a comprehensive overview of various drug classes, including adrenergic blocking agents, ACE inhibitors, calcium channel blockers, and antilipemic. Each medication’s mechanism of action, indications for use, adverse effects, and implications for nursing practice will be thoroughly examined. This chapter draws from knowledge of normal mechanisms of perfusion learned in the previous chapter.
Additionally, we will explore the etiology, pathophysiology, and clinical manifestations of dyslipidemia, along with non-pharmacologic strategies and interventions to enhance therapeutic outcomes. The chapter will also cover the use of antilipemic agents, detailing their mechanisms, indications, and nursing considerations. Finally, we will discuss the rationale behind medication combinations to control hypertension and manage dyslipidemia effectively, highlighting the importance of a holistic approach to cardiovascular care. By understanding these interconnected pathways, you will be better equipped to manage and educate patients on preventing and treating hypertension and dyslipidemia, ultimately improving their cardiovascular health and overall well-being.
Learning Objectives:
- Understand the etiology, pathophysiology, and clinical manifestations of high blood pressure.
- Discuss non-pharmacological measures to control hypertension.
- Explain the mechanism of action, indications for use, adverse effects, and nursing process implications for adrenergic blocking agents, adrenergic receptor stimulators, angiotensin converting enzyme (ACE) inhibitors, calcium channel blockers, angiotensin II receptor blockers, vasodilators and antilipidemics.
- Discuss the uses of medication combination to control hypertension.
- Understand the etiology, pathophysiology and clinical manifestations of dyslipidemia.
- Discuss non-pharmacologic measures to control dyslipidemia and interventions to increase therapeutic effects.
- Explain the mechanism of action, indications for use, adverse effects, and nursing process implications for antilipemic agents.
I. Circulation, Perfusion, and Blood Pressure Defined
“Circulation is the continuous movement of blood throughout the body, driven by the pumping action of the heart.”
Systematic Circulation: Blood Vessels:
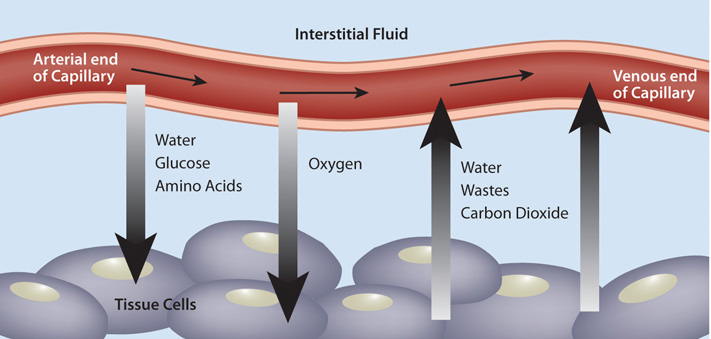
After blood is pumped out of the ventricles, it is carried through the body via blood vessels. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels and eventually into tiny capillaries where nutrients and wastes are exchanged at the cellular level. Capillaries then combine with other small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart. Compared to arteries, veins are thin-walled, low-pressure vessels. Larger veins are also equipped with valves that promote the unidirectional flow of blood toward the heart and prevent backflow caused by the inherent low blood pressure in veins as well as the pull of gravity.
In addition to their primary function of returning blood to the heart, veins may be considered blood reservoirs because systemic veins contain approximately 64 percent of the blood volume at any given time. Approximately 21 percent of the venous blood is located in venous networks within the liver, bone marrow, and integument. This volume of blood is referred to as venous reserve. Through vasoconstriction, this reserve volume of blood can get back to the heart more quickly for redistribution to other parts of the circulation.
Perfusion is the ability of the heart to move oxygen and nutrients throughout the body via the circulatory or lymphatic systems to the capillaries to ensure cellular processes function appropriately. Perfusion is cyclical, meaning that to provide oxygen and nutrients to the cell, the body must also be able to remove cellular wastes and by-products. Inadequate perfusion, also called ischemia, may be the cause of several cardiovascular diseases, including cardiovascular disease, coronary artery disease, cerebrovascular disease, peripheral artery disease, and many other conditions.
Blood Pressure
A blood pressure reading is the measurement of the force of blood against the walls of the arteries as the heart pumps blood through the body. It is reported in millimeters of mercury (mmHg). This pressure changes in the arteries when the heart is contracting compared to when it is resting and filling with blood.
The systolic blood pressure is the maximum pressure on the arteries during systole, the phase of the heartbeat when the ventricles contract (beating). This is the top number of blood pressure readings. Systole causes the ejection of blood out of the ventricles and into the aorta and pulmonary arteries. The diastolic blood pressure is the resting pressure on the arteries during diastole, the phase between each contraction of the heart when the ventricles are filling with blood. This is the bottom number of the blood pressure reading. Therefore, 120/80 indicates the systolic blood pressure is 120 mm Hg, and the diastolic blood pressure is 80 mm Hg.
Many factors can affect blood pressure, such as hormones, stress, exercise, eating, caffeine, heavy alcohol consumption, sitting, and standing. Blood flow through the body is regulated by the size of blood vessels, the action of smooth muscle, one-way valves, and the fluid pressure of the blood itself. Blood Flow and Blood Pressure Regulation.
II. Physiology of Blood Pressure and Pathophysiology of Hypertension
Blood Pressure
Any factor that causes cardiac output to increase, by elevating heart rate or stroke volume or both, will elevate blood pressure and promote blood flow. These factors include sympathetic stimulation, the catecholamines epinephrine and norepinephrine, thyroid hormones, and increased calcium ion levels. Conversely, any factor that decreases cardiac output, by decreasing heart rate, stroke volume, or both, will decrease arterial pressure and blood flow. These factors include parasympathetic stimulation, elevated or decreased potassium ion levels, decreased calcium levels, anoxia, and acidosis. Blood pressure increases with increased cardiac output, peripheral vascular resistance, blood volume, blood viscosity, and rigidity of vessel walls. Blood pressure decreases with decreased cardiac output, peripheral vascular resistance, blood volume, blood viscosity, and vessel wall elasticity.
Blood pressure is influenced by:
- Heart rate (HR) can vary considerably, not only with exercise and fitness levels but also with age. Newborn resting HRs may be 120 -160 bpm. HR gradually decreases until young adulthood and then gradually increases again with age. For an adult, normal resting HR will be in the range of 60–100 bpm. Bradycardia is the condition in which the resting rate drops below 60 bpm, and tachycardia is the condition in which the resting rate is above 100 bpm.
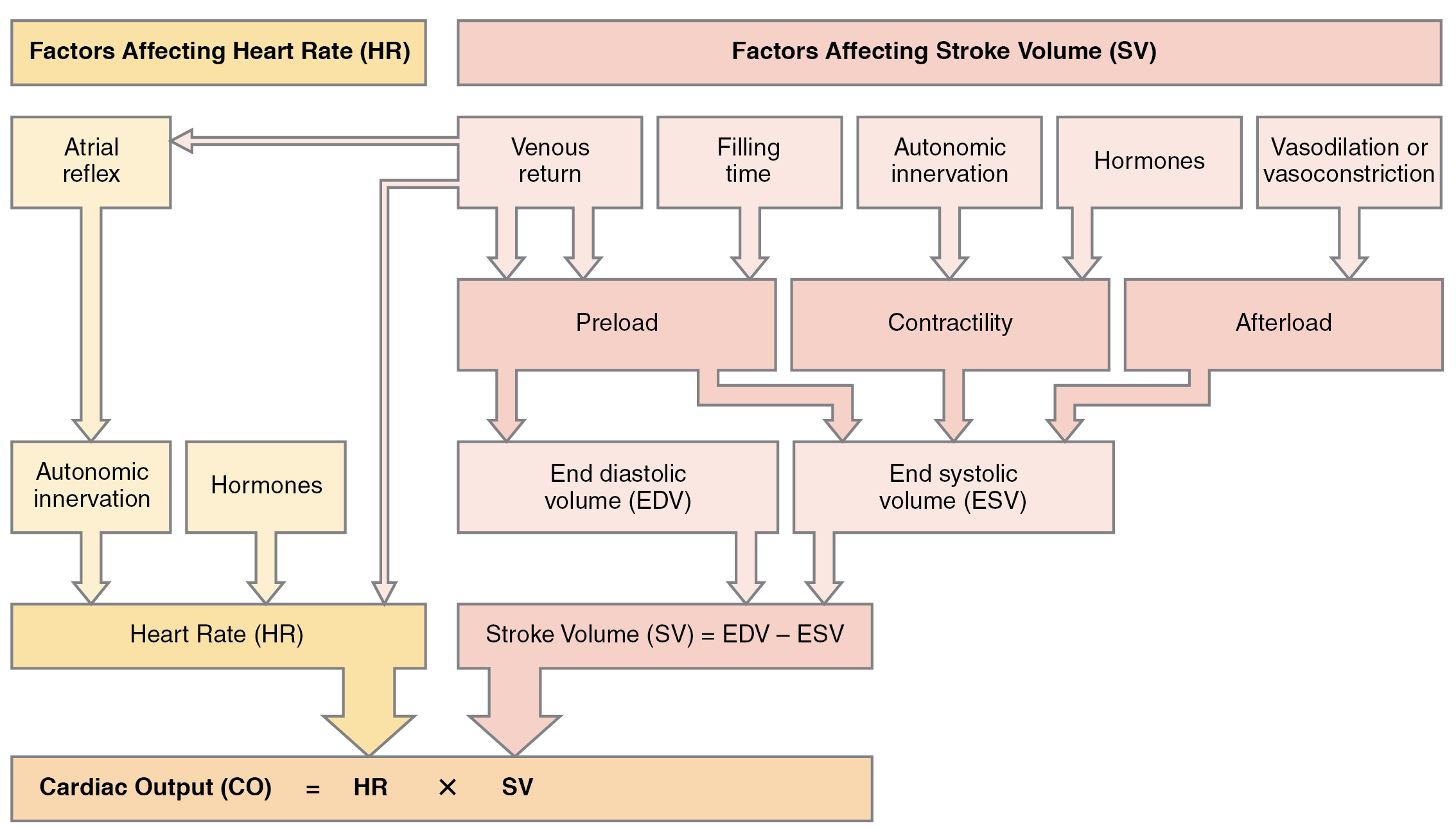
- Stroke volume (SV) is the amount of blood in one clean pump – in other words, what your heart pumps with each beat. It measures how much blood goes through your body every minute. Results depend on the size of the heart and how fast it contracts. Stroke volume (SV) is also used to calculate ejection fraction, the portion of the blood pumped or ejected from the heart with each contraction. Many of the same factors that regulate HR also impact cardiac function by altering SV. Three primary factors affecting stroke volume are preload or the stretch on the ventricles before contraction; contractility, or the force or strength of the contraction itself; and afterload, the force the ventricles must generate to pump blood against the vessel’s resistance. Many cardiovascular medications affect cardiac output by affecting preload, contractility, or afterload.
- Cardiac output (CO) is a measurement of the amount of blood pumped by each ventricle in one minute. To calculate this value, multiply stroke volume (SV), the amount of blood pumped by each ventricle, by the heart rate (HR) in beats per minute. It can be represented mathematically by the following equation: CO = HR × SV. Factors influencing CO include autonomic innervation by the sympathetic and parasympathetic nervous system and hormones such as epinephrine, preload, contractility, and afterload. SV is also used to calculate ejection fraction, the portion of the blood pumped or ejected from the heart with each contraction.

Any factor that causes cardiac output to increase, by elevating heart rate or stroke volume or both, will elevate blood pressure and promote blood flow. These factors include sympathetic stimulation, the catecholamines epinephrine and norepinephrine, thyroid hormones, and increased calcium ion levels. Conversely, any factor that decreases cardiac output, by decreasing heart rate, stroke volume, or both, will decrease arterial pressure and blood flow. These factors include parasympathetic stimulation, elevated or decreased potassium ion levels, decreased calcium levels, anoxia, and acidosis.
- Peripheral vascular resistance refers to compliance, which is the ability of any compartment to expand to accommodate increased content. A metal pipe, for example, is not compliant, whereas a balloon is. The greater the compliance of an artery, the more effectively it is able to expand to accommodate surges in blood flow without increased resistance or blood pressure. Veins are more compliant than arteries and can expand to hold more blood. When vascular disease causes stiffening of arteries (e.g., atherosclerosis or arteriosclerosis), compliance is reduced, and resistance to blood flow is increased. The result is more turbulence, higher pressure within the vessel, and reduced blood flow. This increases the work of the heart.
- Compliance (elasticity of vessel walls) is the ability of any compartment to expand to accommodate increased content. A metal pipe, for example, is not compliant, whereas a balloon is. The greater the compliance of an artery, the more effectively it is able to expand to accommodate surges in blood flow without increased resistance or blood pressure. When vascular disease causes stiffening of arteries, called arteriosclerosis, compliance is reduced, and resistance to blood flow is increased. The result is higher blood pressure within the vessel and reduced blood flow. Arteriosclerosis is a common cardiovascular disorder that is a leading cause of hypertension and coronary heart disease because it causes the heart to work harder to generate a pressure great enough to overcome the resistance.
- Volume of circulating blood: A relationship exists between blood volume, blood pressure, and blood flow. For example, water may merely trickle along a creek bed in a dry season but rush quickly and under great pressure after heavy rain. Similarly, as blood volume decreases, blood pressure and flow decrease, but when blood volume increases, blood pressure and flow increase. Low blood volume, called hypovolemia, may be caused by bleeding, dehydration, vomiting, severe burns, or by diuretics used to treat hypertension. Treatment typically includes intravenous fluid replacement. Excessive fluid volume, called hypervolemia, is caused by the retention of water and sodium, as seen in patients with heart failure, liver cirrhosis, and some forms of kidney disease. Treatment may include the use of diuretics that cause the kidneys to eliminate sodium and water.
Cardiovascular Centers
Sympathetic stimulation increases the heart rate and contractility, whereas parasympathetic stimulation decreases the heart rate. (See Figure 6.2h for an illustration of the ANS stimulation of the heart.) Sympathetic stimulation causes the release of the neurotransmitter norepinephrine (NE), which shortens the repolarization period, thus speeding the rate of depolarization and contraction and increasing the HR. It also opens sodium and calcium ion channels, allowing an influx of positively charged ions.
NE binds to the Beta-1 receptor. Some cardiac medications (for example, beta-blockers) work by blocking these receptors, thereby slowing HR and lowering blood pressure. However, an overdose of beta blockers can lead to bradycardia and even stop the heart.
!["2032 Automatic Innervation.jpg" by OpenStax College is licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology The vagus nerve (parasympathetic] decreases heart rate. Sympathetic cardiac nerves increases heart rate and force of contraction.](https://opentextbc.ca/accessibilitytoolkit/wp-content/uploads/sites/397/2022/05/image7-1.png)
- Contractility refers to the force of the contraction of the heart muscle, which controls SV. Factors that increase contractility are positive inotropic factors, and those that decrease contractility are negative inotropic factors. Not surprisingly, sympathetic stimulation is a positive inotrope, whereas parasympathetic stimulation is a negative inotrope. The drug digoxin is used to lower HR and increase the strength of the contraction. It works by inhibiting the activity of an enzyme (ATPase) that controls the movement of calcium, sodium, and potassium into the heart muscle. Inhibiting ATPase increases calcium in heart muscle, increasing the force of heart contractions. Negative inotropic agents include hypoxia, acidosis, hyperkalemia, and a variety of medications, such as beta-blockers and calcium channel blockers.
- Preload and Afterload- Preload is, in simplest terms, the stretching of ventricles. Ventricles tend to stretch (fill with blood) and squeeze (push out blood) to distribute blood adequately. However, if too much pressure is backed up due to cardiac issues, the ventricles tend to stretch extensively, taking longer to squeeze, resulting in an abnormal contraction. Too much stretch = inability to squeeze properly. Another definition for Preload is another way of expressing end-diastolic volume (EDV). Therefore, the greater the EDV, the greater the preload. One of the primary factors to consider is filling time, the duration of ventricular diastole during which filling occurs. Any sympathetic stimulation to the venous system will also increase venous return to the heart, which contributes to ventricular filling and preload. Medications such as diuretics decrease preload by causing the kidneys to excrete more water, thus decreasing blood volume. Afterload is a fancy word for the pressure required for the left ventricle to force blood out of the body to exert during systole. In other words, it’s the effort of the ventricle squeezing. Afterload refers to the force that the ventricles must develop to pump blood effectively against the resistance in the vascular system. Any condition that increases resistance requires a greater afterload to force open the semilunar valves and pump the blood, which decreases cardiac output. On the other hand, any decrease in resistance reduces the afterload and thus increases cardiac output. Another definition of afterload is the force that the ventricles must develop to pump blood effectively against resistance in the vascular system. Any condition that increases resistance requires a greater afterload to force open the semilunar valves and pump the blood, which decreases cardiac output. On the other hand, any decrease in resistance reduces the afterload and thus increases cardiac output. The figure below summarizes the major factors influencing cardiac output. Calcium channel blockers such as amlodipine, verapamil, nifedipine, and diltiazem can be used to reduce afterload and thus increase cardiac output.
Below is a summary of the major factors influencing cardiac output. Calcium channel blockers such as amlodipine, verapamil, nifedipine, and diltiazem can reduce afterload and thus increase cardiac output.
- Viscosity of blood is a measure of the blood’s thickness and is influenced by the presence of plasma proteins and formed elements. Blood is viscous and somewhat sticky to the touch. It has a viscosity approximately five times greater than water. Viscosity is a measure of a fluid’s thickness or resistance to flow and is influenced by the presence of plasma proteins and formed elements within the blood. The viscosity of blood has a dramatic effect on blood pressure and flow. Consider the difference in flow between water and honey. The more viscous honey would demonstrate a greater resistance to flow than the less viscous water. The same principle applies to blood.
- Elasticity of vessel walls refers to the capacity to resume normal shape after stretching and compressing. Vessels larger than 10 mm in diameter are typically elastic. Their abundant elastic fibers allow them to expand as blood pumped from the ventricles passes through them and recoil after the surge. If artery walls were rigid and unable to expand and recoil, their resistance to blood flow would greatly increase. Blood pressure would rise to even higher levels, requiring the heart to pump harder to increase the volume of blood expelled by each pump (the stroke volume) and maintain adequate pressure and flow. Artery walls would have to become even thicker in response to this increased pressure.
Other factors that affect blood pressure:
- A. Homeostatic Regulation of the Cardiovascular System: To maintain homeostasis in the cardiovascular system and provide adequate blood to the tissues, blood flow must be redirected continually to the tissues as they become more active. For example, when an individual exercises, more blood will be directed to skeletal muscles, the heart, and the lungs. On the other hand, following a meal, more blood is directed to the digestive system. Only the brain receives a constant blood supply regardless of rest or activity. Three homeostatic mechanisms ensure adequate blood flow and, ultimately, perfusion of tissues: neural, endocrine, and autoregulatory mechanisms.
- Neural Regulation: The nervous system is critical in regulating vascular homeostasis based on baroreceptors and chemoreceptors. Baroreceptors are specialized stretch receptors located within the aorta and carotid arteries that respond to the degree of stretch caused by the presence of blood and then send impulses to the cardiovascular center to regulate blood pressure. In addition to the baroreceptors, chemoreceptors monitor levels of oxygen, carbon dioxide, and hydrogen ions (pH). When the cardiovascular center in the brain receives this input, it triggers a reflex that maintains homeostasis.
- Endocrine Regulation: Endocrine control over the cardiovascular system involves catecholamines, epinephrine, and norepinephrine, as well as several hormones that interact with the kidneys to regulate blood volume.
- Epinephrine and Norepinephrine: The catecholamines epinephrine and norepinephrine are released by the adrenal medulla and are a part of the body’s sympathetic or fight-or-flight response. They increase heart rate and force of contraction while temporarily constricting blood vessels to organs not essential for fight-or-flight responses and redirecting blood flow to the liver, muscles, and heart.
- Antidiuretic Hormone: The hypothalamus secretes antidiuretic hormone (ADH), also known as vasopressin. The primary trigger prompting the hypothalamus to release ADH is increasing the osmolarity of tissue fluid, usually in response to a significant loss of blood volume. ADH signals its target cells in the kidneys to reabsorb more water, thus preventing additional fluid loss in the urine. This will increase overall fluid levels and help restore blood volume and pressure.
- The renin-angiotensin-aldosterone system(RAAS) has a major effect on the cardiovascular system. Specialized kidney cells respond to decreased blood flow by secreting renin into the blood. Renin converts the plasma protein angiotensinogen into its active form—Angiotensin I. Angiotensin I circulates in the blood and is then converted into Angiotensin II in the lungs. This reaction is catalyzed by the enzyme called angiotensin-converting enzyme (ACE). ACE inhibitors, such as lisinopril, target this step in the RAAS to decrease blood pressure.
Angiotensin II is a powerful vasoconstrictor that greatly increases blood pressure. It also stimulates the release of ADH and aldosterone, a hormone the adrenal cortex produces. Aldosterone then increases the kidneys’ reabsorption of sodium into the blood. Because water follows sodium, there is an increase in the reabsorption of water, which increases blood volume and blood pressure. The illustration of the renin-angiotensin-aldosterone system and the figure below summarize the effect of hormones involved in renal control of blood pressure.
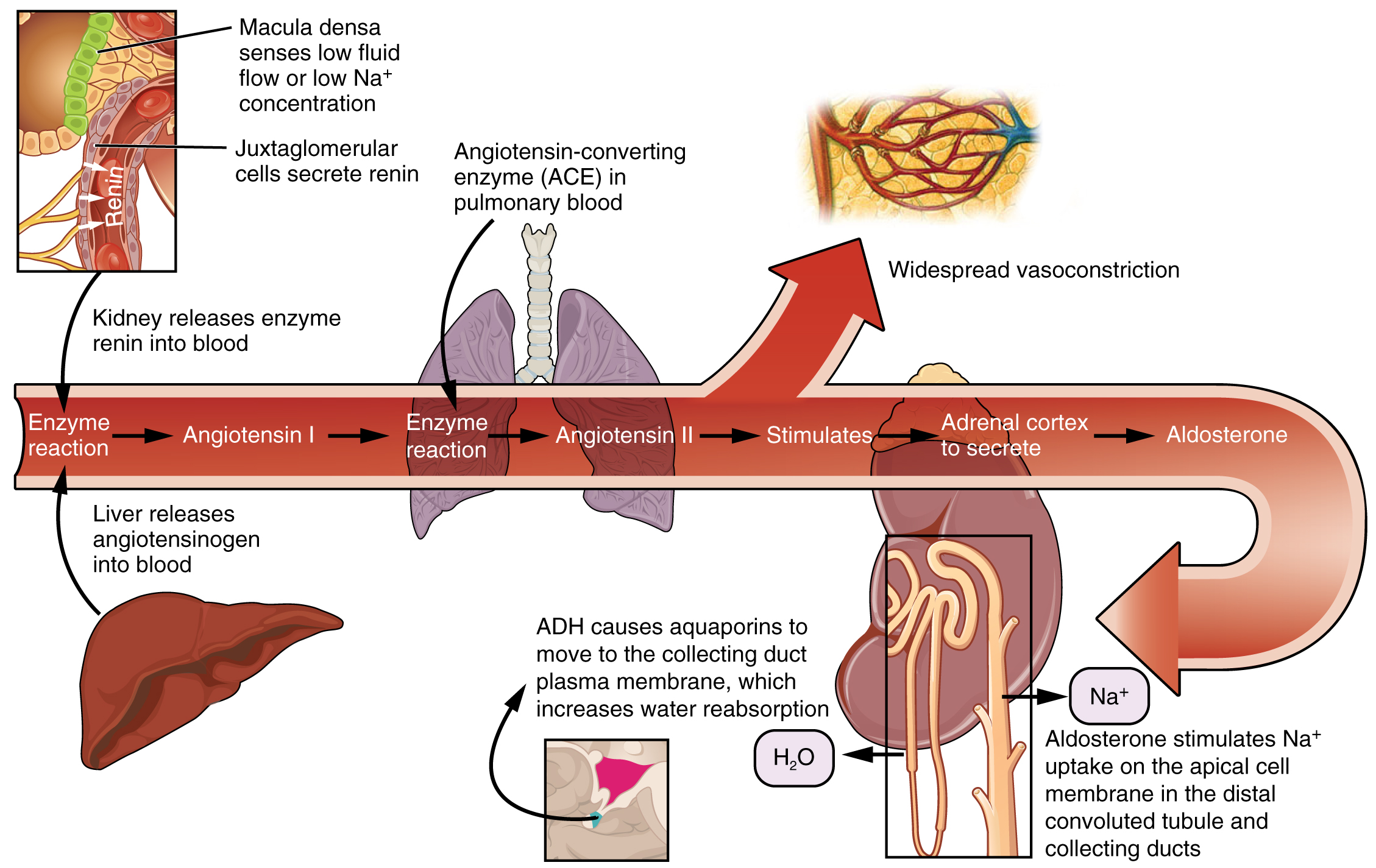
Above: The renin-angiotensin-aldosterone system
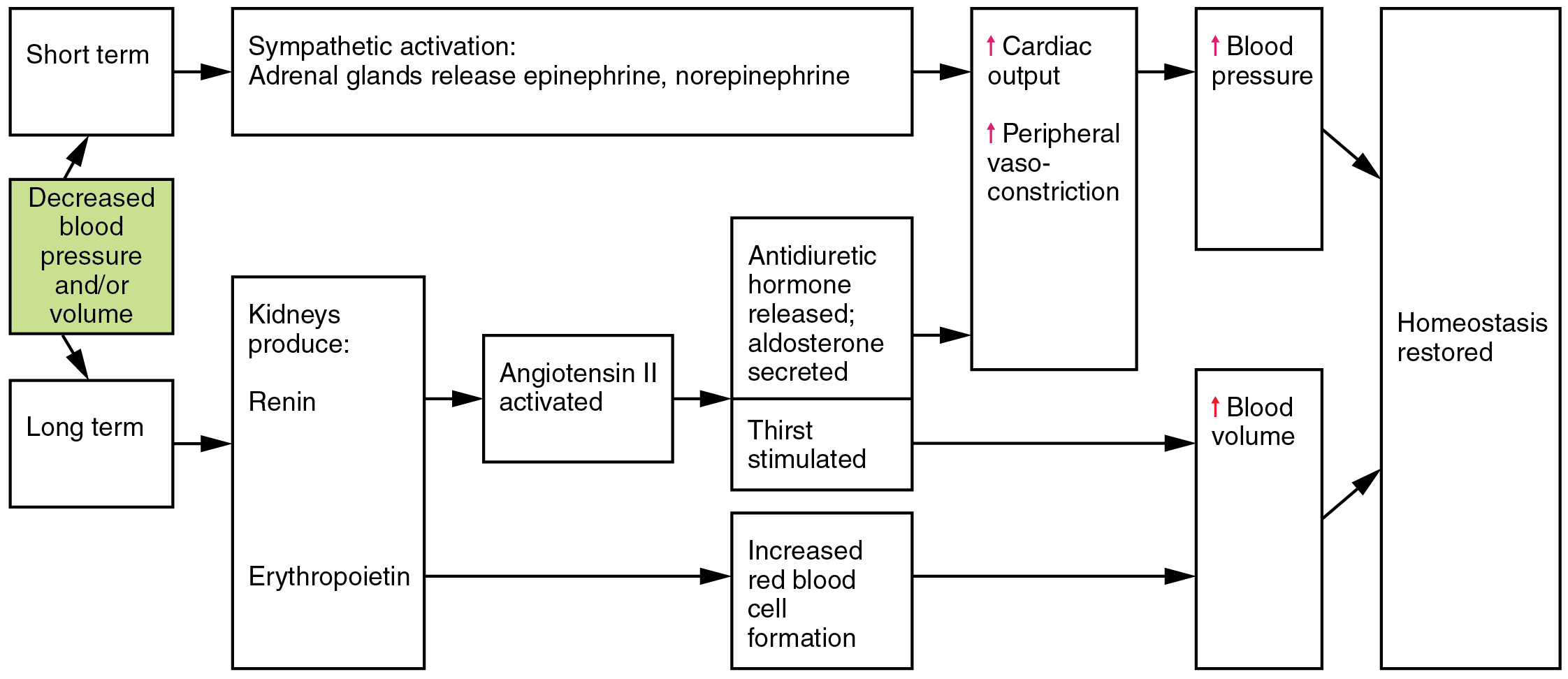
Hormones involved in renal control of blood pressure
Autoregulation of Perfusion
Local, self-regulatory mechanisms allow each region of tissue to adjust its blood flow—and thus its perfusion. These mechanisms are affected by sympathetic and parasympathetic stimulation and endocrine factors. See the figure below for a summary of these factors and their effects.
| Control | Factor | Vasoconstriction | Vasodilation |
| Neural | Sympathetic stimulation | Arterioles within integument abdominal viscera and mucosa membrane; skeletal muscles (at high levels); varied in veins and venules | Arterioles within the heart; skeletal muscles at low to moderate levels |
| Parasympathetic | No known innervation for most | Arterioles in external genitalia; no known innervation for most other arterioles or veins | |
| Endocrine | Epinephrine | At high levels, it is similar to sympathetic stimulation for extended fight-or-flight responses, binding to specialized alpha (α) receptors. | Similar to sympathetic stimulation for extended fight-or-flight responses, at low to moderate levels, it binds to specialized beta (β) receptors. |
| Norepinephrine | Similar to epinephrine | Similar to epinephrine | |
| Angiotensin II | Powerful generalized vasoconstrictor; also stimulates the release of aldosterone and ADH | n/a | |
| ANH (peptide) | n/a | A powerful generalized vasodilator also promotes kidney fluid loss, reducing blood volume, pressure, and flow. | |
| ADH | Moderately strong generalized vasoconstrictors also cause the body to retain more fluid via the kidneys, increasing blood volume and pressure | n/a | |
| Other factors | Decreasing levels of oxygen | n/a | Vasodilation also opens precapillary sphincters |
| Decreasing pH | n/a | Vasodilation also opens precapillary sphincters | |
| Increasing levels of carbon dioxide | n/a | Vasodilation also opens precapillary sphincters | |
| Increasing levels of potassium ion | n/a | Vasodilation also opens precapillary sphincters | |
| Increasing levels of prostaglandins | Vasoconstriction closes precapillary sphincters | Vasodilation opens precapillary sphincters | |
| Increasing levels of adenosine | n/a | Vasodilation | |
| Increasing levels of lactic acid and other metabolites | n/a | Vasodilation also opens precapillary sphincters | |
| Increasing levels of endothelins | Vasoconstriction | n/a | |
| Increasing levels of platelet secretions | Vasoconstriction | n/a | |
| Increasing hypothermia | n/a | Vasodilation | |
| Stretching of the vascular wall (myogenic) | Vasoconstriction | n/a | |
| Increasing levels of histamines from basophils and mast cells | n/a | Vasodilation |
The effects of nervous, endocrine, and local controls on the vasoconstriction and vasodilation of arterioles
III. Blood Pressure and Hypertension
Blood pressure measurements are obtained using a stethoscope and a sphygmomanometer, also called a blood pressure cuff. To obtain a manual blood pressure reading, the blood pressure cuff is placed around a patient’s extremity, and a stethoscope is placed over an artery. For most blood pressure readings, the cuff is usually placed around the upper arm, and the stethoscope is placed over the brachial artery. The cuff is inflated to constrict the artery until the pulse is no longer palpable and then deflated slowly. The American Heart Association (AHA) recommends that the blood pressure cuff be inflated at least 30 mmHg above the point where the radial pulse is no longer palpable. The first appearance of sounds, called Korotkoff sounds, is noted as the systolic blood pressure reading. Korotkoff sounds are named after Dr. Korotkoff, who first discovered the audible sounds of blood pressure when the arm is constricted. The blood pressure cuff continues to be deflated until Korotkoff sounds disappear. The last Korotkoff sounds reflect the diastolic blood pressure reading. It is important to deflate the cuff slowly at no more than 2-3 mmHg per second to ensure that the absence of pulse is noted promptly and that the reading is accurate. Blood pressure readings are documented as systolic/diastolic pressure, for example, 120/80 mmHg.
Abnormal blood pressure readings can signify an area of concern and a need for intervention. Normal adult blood pressure is less than 120/80 mmHg. Hypertension is the medical term for elevated blood pressure readings of 130/80 mmHg or higher. See Table 3.2 for blood pressure categories according to the 2017 American College of Cardiology and American Heart Association Blood Pressure Guidelines. Before diagnosing a person with hypertension, the healthcare provider will calculate an average blood pressure based on two or more blood pressure readings obtained on two or more occasions.
Hypotension is the medical term for low blood pressure readings less than 90/60 mmHg. It can be caused by dehydration, bleeding, cardiac conditions, and the side effects of many medications. Hypotension can be of significant concern because it can lead to a potential lack of perfusion to critical organs.
Orthostatic hypotension is a drop in blood pressure that occurs when moving from a lying down (supine) or seated position to a standing (upright) position. When measuring blood pressure, orthostatic hypotension is defined as a decrease in blood pressure by at least 20 mmHg systolic or 10 mmHg diastolic within three minutes of standing. When a person stands, gravity moves blood from the upper body to the lower limbs. As a result, there is a temporary reduction in the amount of blood in the upper body for the heart to pump, which decreases blood pressure. Typically, the body quickly counteracts the force of gravity and maintains stable blood pressure and blood flow. In most people, this transient drop in blood pressure goes unnoticed. However, some patients with orthostatic hypotension can experience light-headedness, dizziness, or fainting. This is a significant safety concern because of the increased risk of falls and injury, particularly in older adults. Orthostatic hypotension is also commonly referred to as postural hypotension. When obtaining orthostatic vital signs, the pulse rate may also be collected. If the pulse increases by 30 beats/minute or more while the patient stands (or sits if unable to stand), this indicates a significant change.
Orthostatic Vital Signs
Perform the following actions when obtaining orthostatic vital signs:
- Have the patient stand upright for 1 minute if able.
- Obtain the blood pressure measurement while the patient stands using the same arm and equipment as the previous measurement taken with the patient lying or sitting.
- Obtain the radial pulse again.
- Repeat the blood pressure and radial pulse measurements at 3 minutes. Waiting several minutes before repeating the measurements allows the autonomic nervous system to compensate for blood volume shifts after a position change in the patient without orthostatic hypotension.
- Repeat blood pressure measurement if the patient has symptoms that suggest orthostatic hypotension but don’t have documented orthostatic hypotension.
Tip: Some patients may not demonstrate significant decreases in blood pressure until standing for more than 3 minutes.
- Therefore, adequate time is needed when testing for orthostatic blood pressure as the patient is at risk for falls.
Equipment to Measure Manual Blood Pressure
A sphygmomanometer, commonly called a blood pressure cuff, measures blood pressure while Korotkoff sounds are auscultated using a stethoscope. Below is an image of a sphygmomanometer and stethoscope.
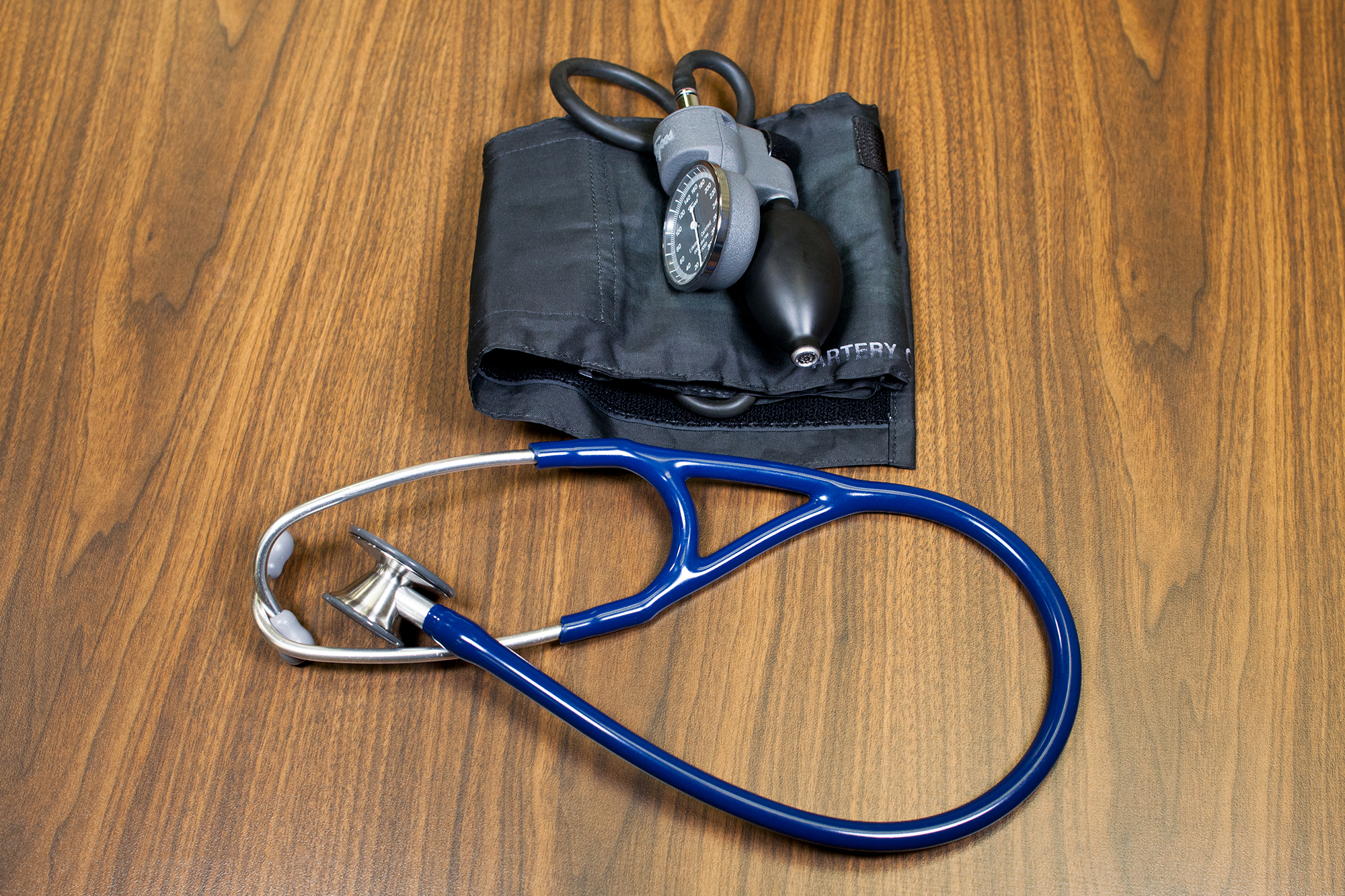
There are various sizes of blood pressure cuffs. It is crucial to select the appropriate size for the patient to obtain an accurate reading. An undersized cuff will produce an artificially high reading, and an oversized cuff will create an artificially low reading.
Cuff Types and Sizes
Manual and automatic blood pressure measurement involves using a blood pressure cuff with a sphygmomanometer. Many cuff sizes are available to fit newborns, children, adults, people with small and larger arms, and people with cone-shaped arms. The cuff is typically wrapped around the upper arm. However, a cuff can also be placed on the thigh when the arm is not feasible. When taking the measurement, ensure that the arm and wrist are supported at heart level (Nerenberg, 2018).

Automatic blood pressure cuffs are a digital way to measure blood pressure. After positioning the patient and the blood pressure cuff on the arm, press the start button on the monitor. The cuff is automatically inflated and deflates at 2 mm Hg per second. The monitor has a digital display that shows the blood pressure reading when done. Automatic cuffs can be programmed to take a series of blood pressure readings in a row. If the healthcare provider is concerned about an initial high blood pressure reading on a patient, the accuracy of the blood pressure is verified with the following actions:
- Have the patient sit in a room by themselves
- Quiet the room
- Dim the lights
- Allow the patient to sit quietly without talking
- Then, take three measurements, a few minutes apart, with the automatic cuff. The blood pressure displayed is an average of the three readings.

Patients can monitor their own blood pressure at home with an automatic digital blood pressure monitoring device. The cuff is applied around the patient’s upper arm or wrist. Like the automatic cuff noted above, the patient presses the start button, and the cuff inflates and deflates based on programmed levels displaying a digital reading. Patients are encouraged to document their blood pressure or use a device with data-recording capabilities to increase the reliability of their reported home blood pressure monitoring. These data can be shared with the patient’s primary care provider.
Arterial catheters are an invasive way to measure blood pressure. They are only used in critical care situations when continuous blood pressure monitoring and arterial blood gas draws are required. The procedure involves inserting a catheter (similar to an intravenous) into the artery. The catheter is connected to a pressure transducer and monitor that provides a digital blood pressure reading.
Cellular phone applications have been developed to measure blood pressure, but the accuracy of this technology is still being investigated.
Definition of Hypertension: High blood pressure, or hypertension, “is when the force of the blood pushing on the blood vessel walls is too high.”
Risk factors for Hypertension:
The healthcare provider assesses a patient’s cardiovascular risk factors for atherosclerosis and hypertension. These risk factors are categorized as modifiable and non-modifiable. See below for resources concerning risk factors based on “Hypertension Canada guidelines (Leung et al., for Hypertension Canada, 2017)” and “What causes Hypertension- Risk factors:”https://storymd.com/journal/pwvvoz507w-high-blood pressure/page/lzazr1lxka-high-blood-pressure-risk-factors
| Non-modifiable | Modifiable |
| Age
Men over 50 and post-menopausal women |
Too high sodium. sugar, and fat/cholesterol intake
Deficits in Magnesium and potassium intake |
| Race/ethnicity
African Americans and Hispanics have a higher incidence rate of HTN than whites. |
Inactivity-sedentary lifestyle, Diabetes, and dyslipidemia |
| Family history | Obesity, especially abdominal obesity |
| Greater consumption of alcohol and caffeine | |
| Sleep deprivation/sleep apnea | |
| Smoking, Stress, and anxiety | |
| Meds: Aspirin, NSAIDs, ibuprofen, anti-depressants, decongestants, hormonal birth control | |
| Medical conditions:
|
|
| Social-economical disparities: Non-adherence to lifestyle or medication plan
Income, education, location of housing, and profession/job type |
Unfolding Case Study for Hypertension:
Part A
Sharon Jones (SJ) is a 40-year-old African American female. She is 65 inches tall and weighs 220 pounds. She came to her Primary Care Provider (PCP) for her first physical in five years:
History and Physical (H & P)
Allergies: Bactrim, which leads to shortness of breath, and bee venom, which leads to swelling of the face and lips; denies food allergies.
PMH: Obesity since childhood, grew up with secondhand cigarette smoke in the home
Activity: exercises with a Jazzercise class every Saturday-does not exercise after walking around the library on weekdays
PSH: Appendectomy at the age of 12
FH: Mother has Hypertension (HTN), and Asthma; Father and all paternal relatives have been diagnosed with Diabetes Mellitus (DM) type 2, and Acid Reflux
Social History:
Drinks two glasses of wine when out with friends on weekends, denies use of Illicit drugs, including marijuana, but smokes a cigarette occasionally when feeling stressed. Spends Sunday afternoons at parents’ house with the parents and the families of her three brothers. Attends church services most Sundays. She is Methodist.
Medications: Multi-vitamin (MVI) one tab po once daily and Yaz 1 tab po once daily in the morning (birth control)
Occupation: Librarian who works 50 hours a week
Hobbies: Volunteers as a den mother for her neighborhood Girl Scout troop.
Review of Systems: The patient denies any complaints about any body system except for new mild tachypnea, fatigue after long episodes of strenuous exercise, and an inability to sleep well and wake up fully rested.
Questions to test newly obtained knowledge from the OER:
- What risk factors does SJ have for hypertension?
- What further data would the healthcare team use to initiate a plan of care for hypertension?
Blood Pressure Categories
| Blood Pressure Category | Systolic mm Hg | Diastolic mm Hg |
| Normal | Less than 120 | Less than80 |
| Elevated | 120-129 | Less than 80 |
| Stage 1 | 130-139 | 80-89 |
| Stage 2 | 140 or higher | Greater or equal to 90 |
| Hypertensive Crisis | Greater than 180 | Greater than 120 |
In 2017, new guidelines from the American Heart Association, the American College of Cardiology, and nine other health organizations lowered the numbers for the diagnosis of hypertension (high blood pressure) to 130/80 millimeters of mercury (mm Hg) and higher for all adults. The previous guidelines set the threshold at 140/90 mm Hg for people younger than age 65 and 150/80 mm Hg for those ages 65 and older.
Management of Hypertension is crucial as uncontrolled hypertension may lead to:
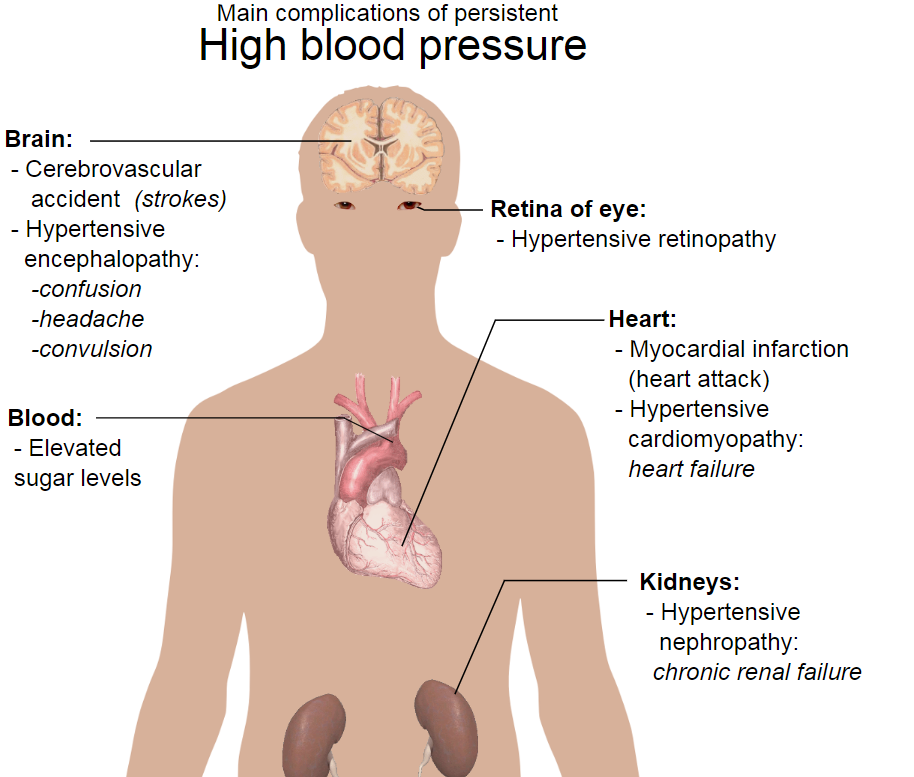
Damage to other organs includes:
Cardiac: Artery damage, hardened arteries, aneurysms, arrhythmias, chest pain, heart disease, heart attack, stroke
Cognitive problems: memory and understanding and possible dementia, anxiety, depression
Neurological problems: Sexual dysfunction, loss of vision
Musculoskeletal: Bone loss and Osteoporosis
Genitourinary: Renal disease and hormone problems
Other: Sleep apnea and blood clots
IV. Management of Hypertension. Non-Pharmacological Interventions and Antihypertensive Medication
Non-pharmacological Interventions
Lifestyle changes that will improve the health of a patient with hypertension include:
- Weight loss
- Mediterranean/DASH diet: https://en.wikipedia.org/wiki/MIND_diet
- Decrease sodium, sugar, and fat intake
- Moderate exercise for 30-60 minutes several times a week.
- Stop smoking
- Limit alcohol and caffeine intake
- Stress management
- Appropriate sleep and address sleep apnea
- Self-monitoring of blood pressure
Exercises: Unfolding Case Study Part B
Sharon Jones’s (SJ) physical assessment starts with obtaining vital signs: T 98°F, P 70 bpm, 18 bpm, 145/88 mmHg
The patient was unaware that her blood pressure was elevated
The physical assessment findings:
She is alert and oriented x4 and comprehends all questions and statements well. Cranial nerves II-VII are grossly intact, but on her last eye exam, there were minimal changes to the optic nerve. Sleeps 4-6 hours per night but does not awake rested, and her neck is short and thick. Upper and lower extremity strength is 5/5 and movements are coordinated, active ROM noted to all four extremities. Lower back pain of 2/10 noted with repeated bending to touch toes. The pain was relieved when the repeated bending stopped. Skin intact with slight edema noted to ankles. Skin intact throughout the body. S1 and S2 were noted without ectopy with regular rate and rhythm. Thorax is normal in shape and size. Lung sounds are clear throughout lung fields with regular rate, rhythm, and depth. The abdomen is soft, non-distended, and non-tender, with positive bowel sounds to all four quadrants with BM every morning. The urine sample indicates clear yellow urine with an aromatic odor.
- What data in the physical assessment findings indicates that SJ has hypertension?
- What stage of hypertension is the patient in?
- What non-pharmacological interventions are recommended now?
VI. Antihypertensive Medications
Many different medication classifications are used to treat hypertension. Understanding the different mechanisms of action for different classes of anti-hypertensives is important because patients are often on a combination of medications that work synergistically to manage blood pressure.
- Alpha-2 Agonist
Clonidine is an Alpha-2 agonist.
Alpha-2 Agonist
Mechanism of Action: Clonidine stimulates the alpha-adrenergic receptors, resulting in vasodilation and decreased blood pressure. Thus, it decreases peripheral resistance, increases blood flow to the kidneys, and decreases afterload.
Indications for Use: Clonidine is used to treat hypertension and can also be used for Attention-Deficit/Hyperactivity Disorder (ADHD) in an extended release version. This medication can be administered in an oral form and a transdermal patch.
Nursing Considerations Across the Lifespan: Monitor BP and pulse rate. Dosage is usually adjusted to the patient’s blood pressure because it can cause hypotension, bradycardia, and sedation.
Rebound hypertension may occur if stopped abruptly.
Patient Teaching and Education: Patients should be compliant with medication therapy. Compliance includes: taking the medication at the same time each day, being careful not to take more than the prescribed dose within a 24-hour period, and avoid stopping medication abruptly, as sudden stoppage may leads to rebound hypertension.
- Medications may cause orthostatic changes, so individuals should change positions slowly. Additionally, medications may cause dry mouth and dry eyes. Individuals should also avoid the use of alcohol and other CNS depressants while taking these medications.
2. Ace Inhibitor (Angiotensin Converting Enzyme)
Captopril is an example of an ACE (angiotensin-converting enzyme) inhibitor.
ACE Inhibitors
Mechanisms of Action: This medication blocks the conversion of Angiotensin I to Angiotensin II in the renin-angiotensin-aldosterone system. Blocking aldosterone will lead to vasodilation and sodium and water excretion.
Indications for Use: Captopril is used to treat hypertension and heart failure. This medication also helps reduce diabetic nephropathy.
Nursing Considerations Across the Lifespan: Do not administer to patients who are pregnant. Use with caution with patients who have diabetes.
Avoid the use of other medications that increase potassium. This medication may increase the risk of lithium toxicity.
Adverse/Side Effects: Black Box Warning: Patients who become pregnant should discontinue this medication due to the risk of fetal harm or fetal death.
Patients taking this medication may experience hypotension, cough, hyperkalemia, increased risk of infection, angioedema, anaphylactoid reactions, or proteinuria. Patients who experience increased facial swelling or difficulty swallowing or breathing should seek emergency medical attention. Report a persistent cough or angioedema to the health care provider.
Patient Teaching and Education: Medications should be taken as directed. Patients taking ACE inhibitors should be cautioned to avoid salt substitutes or foods high in potassium. Additionally, the medication may alter the sense of taste, but this generally resolves within 2-3 months of medication therapy.
Patients taking ACE inhibitors may also experience a persistent cough throughout the duration of medication therapy.
3. Angiotensin II Receptor Blocker (ARB)
Losartan is an example of an Angiotensin II receptor blocker, also known as an ARB. ARBs are similar to ACE inhibitors in that they act on the renin-angiotensin-aldosterone system (RAAS). However, the difference is that they block Angiotensin II and cause vasodilation and decreased peripheral resistance, but they are not likely to cause the cough that ACE inhibitors can.
ARB
Mechanism of Action: Losartan blocks Angiotensin II in the renin-angiotensin-aldosterone system to produce vasodilation.
Indications for Use: ARB is used to treat hypertension and to prevent nephropathy in diabetic patients.
Nursing Considerations Across the Lifespan: Do not administer to patients who are pregnant. It is not recommended for children under 6. Anticipate dosage adjustment with hepatic impairment. This drug can cause renal impairment and hyperkalemia.
Adverse/Side Effects: Black Box Warning: Patients who become pregnant should discontinue this medication due to the risk of fetal harm or fetal death.
Patients taking this medication may experience hypotension, dizziness, increased risk of infection, angioedema, or proteinuria. Patients who experience increased facial swelling or difficulty swallowing or breathing should seek emergency medical attention.
Patient Teaching and Education: Medications should be taken as directed, at the same time each day. Patients should not discontinue therapy unless directed to do so by their healthcare provider. Patients should be careful to avoid salt substitutes and foods with high potassium levels. ARBs may cause orthostatic changes, and patients should be cautioned to change positions slowly.
4. Vasodilator
Hydralazine is an example of a direct vasodilator.
Another example of a vasodilator is Nitroglycerin, which causes arterial and venous vasodilation. It is used for patients with angina to decrease cardiac workload and increase the amount of oxygen available to the heart. By causing vasodilation of the veins, nitroglycerin decreases the amount of blood returned to the heart and thus decreases preload. It also reduces afterload by causing vasodilation of the arteries and reducing peripheral vascular resistance. By reducing preload and afterload, Nitroglycerin is also used as an antihypertensive medication.
Vasodilator
Mechanism of Action: vasodilation via direct relaxation of vascular smooth muscle. Peripheral vasodilation reduces blood pressure and decreases vascular resistance, resulting in increased cardiac output. The direct mechanism of Hydralazine is unknown.
Indications for Use: Vasodilators are used to treat hypertension.
Nursing Considerations Across the Lifespan: Use with caution in patients with coronary artery disease, mitral valve rheumatic heart disease, and cerebral vascular accidents. This medication should only be used in pregnancy if the benefits outweigh the risks due to a lack of safety studies.
Adverse/Side Effects:
Patients should be monitored for infection and are at risk of developing systemic lupus erythematosus (SLE). SLE is a chronic disease that causes inflammation in connective tissues. The signs and symptoms of SLE vary among affected individuals. They can involve many organs and systems, including the skin, joints, kidneys, lungs, central nervous system, and blood-forming (hematopoietic) system. A characteristic sign of SLE is a flat, red rash across the cheeks and bridge of the nose. This rash is called a “butterfly rash” because of its shape.
Hypotension, palpitations, angina, tremors, numbness, tingling, disorientation, nasal congestion, headache, nausea, vomiting, and diarrhea are effects associated with hydralazine.
Patient Teaching & Education: Patients should comply with the therapeutic dosing regimen, even if symptoms resolve. They should be cautious not to double up on medication doses. Additionally, if two or more doses of medication are missed, the patient should consult the healthcare provider for follow-up instruction. Patients should be instructed to monitor their weight and assess for fluid retention in the feet and ankles. Additionally, the medication can cause side effects of orthostatic hypotension and drowsiness.
5. Beta-1 Antagonist
Metoprolol is a selective Beta-1 blocker.
Beta-1 Antagonist
Mechanism of Action: Metoprolol primarily blocks beta-1 receptors in the heart, causing decreased heart rate and blood pressure. However, higher doses can also block beta-2 receptors in the lungs, causing bronchoconstriction.
Indication of Use: Metoprolol is commonly used to treat high blood pressure, chest pain due to poor blood flow to the heart, and several heart conditions involving an abnormally fast heart rate. It is also used as an early intervention during myocardial infarction (MI) to reduce the heart’s workload.
Nursing Considerations Across the Lifespan: ER formulations should not be crushed. Assess the patient’s apical pulse rate before administering; if it is less than 60 beats/minute, withhold the drug and call the prescriber immediately unless other parameters are provided. In diabetic patients, monitor glucose levels closely because the drug masks common signs and symptoms of hypoglycemia.
Adverse/Side Effects: The most serious potential adverse effects are shortness of breath, bradycardia, and worsening heart failure. Other adverse effects include fatigue, dizziness, depression, insomnia, nightmares, GI upset, erectile dysfunction, dyspnea, and wheezing. Black Box Warning: When stopping therapy, taper dosage over 1 to 2 weeks because abrupt discontinuation may cause chest pain or MI.
Patient Teaching & Education: Patients should comply with medication therapy and take the medication simultaneously daily. Do not abruptly cease medication, as arrhythmias, hypertension, or ischemia may develop. Patients and their families should be instructed to check pulse and blood pressure and report abnormalities to the healthcare provider. Additionally, these medications may cause side effects of dizziness and cold sensitivity
6. Class II-Beta Blocker
Class II medications are beta blockers used to decrease conduction velocity, automaticity, and the refractory period of the cardiac conduction cycle. Sotalol is a Beta-1 and Beta-2 blocker with Class III antiarrhythmic properties.
Sotalol is an example of a drug that is both a Beta-1 and Beta-2 blocker but is also a Class III antiarrhythmic properties.
Class II-Beta Blocker-Patient will need cardiovascular monitoring
Mechanism of Action: Sotalol is a non-selective beta-adrenergic blocker that prolongs the cardiac action potential.
Implication of Use: Sotalol is given to patients with life-threatening arrhythmias, such as ventricular or supraventricular arrhythmias. It is not recommended for patients with less-than-severe arrhythmias.
Nursing Considerations Across the Lifespan: Titration of this medication is done by evaluating renal function and monitoring QTc on the ECG 2-4 hours after each medication’s initiation. Patients with decreased renal function require dosage adjustment. Sotalol is contraindicated for patients with decreased serum potassium, bradycardia, 2nd—or 3rd-degree heart block, heart failure, and conditions leading to bronchospasm.
Adverse/Side Effects: Black Box Warning: This drug can cause arrhythmias. This medication lengthens a patient’s QTc interval. Initiation of this medication requires a patient to be in a facility to determine baseline QT and intermittent QT interval checks. QT interval checks are done 2-4 hours after each dose. If the QT corrected interval is greater than 500 msec, the dosing must be changed.
Common side effects of sotalol are arrhythmias, chest pain, palpitations, fatigue, dizziness, hypotension, bradycardia, heart failure, cardiac ischemia, bronchospasm, thyroid abnormalities, and hypoglycemia.
Patient Teaching & Education: Patients should be instructed regarding the significance of compliance with therapeutic drug regimens and should take medications as prescribed, even if not symptomatic. Patients or family members may need instructions on taking pulse rate and blood pressure. They should receive parameters regarding reporting to their healthcare provider. They should report any pulse rate of less than 60 bpm and significant changes in blood pressure.
Patients should also be advised that these medications may cause dizziness and visual changes. They may also notice orthostatic blood pressure decrease with position changes and should be advised to change positions slowly. If the patient notices an irregular, fast heart rate or experiences any fainting episodes, they should notify their healthcare provider immediately.
Additionally, these medications may also mask the signs of hypoglycemia, so diabetic patients must use extra caution to monitor for low blood sugar. These medications may also increase cold sensitivity.[1]
An Example of a drug card: Metoprolol Medication Card
Medication Card: Metoprolol
Class: Antihypertensives– Beta 1 Antagonists, also called beta-blockers
Prototypes: Metoprolol
Mechanism: Metoprolol primarily blocks Beta-1 receptors in the heart, causing decreased heart rate and decreased blood pressure. However, higher doses can also block Beta-2 receptors in the lungs, causing bronchoconstriction.
Therapeutic Effects
- Decrease the workload of the heart
- Decreases blood pressure
- Decreases Heart Rate
Administration
- Do not crush medications
- Assess heart rate and hold medication if HR is less than 60 beats per minute.
- Monitor blood pressure daily and report abnormal BP and HR to MD
- Take as ordered at the same time every day
Indications
- High blood pressure
- Chest pain in people with poor blood flow to the heart
- Tachycardia and rapid arrhythmias
- Early intervention for myocardial infarction to decrease the workload of heart
Contraindications
- Asthma or respiratory diseases can be affected with the higher dose when beta 2 is stimulated, resulting in cough
Side Effects
- Fatigue
- Dizziness
- Depression
- Insomnia
- Nightmares
- GI upset
- Erectile dysfunction
- Dyspnea
- Wheezing
- Cold sensitivity
- SAFETY: When tapering dosage, do it slowly over a few weeks. The abrupt drop can cause chest pain and MI
Nursing Considerations
- Commonly masks hypoglycemia, so check diabetic blood sugars regularly
Exercise: Unfolding Case Study Part C
The plan of care for Sharon Jones was initiated with non-pharmacological measures. Six months later, she is 190 lbs. and her vital signs are: T: 98 °F, P: 77 bpm, R: 16 bpm, 132/80 mmHg
She has kept a food journal indicating that she eats more fruits and vegetables with each meal as she uses the DASH to manage her blood pressure. As noted above, she has lost 30 lbs. in 6 months and reports exercising four times a week for an hour. Three days a week, she completes a one-hour Jazzercise class, and one day a week, she lifts weights.
An updated H & P:
History: The slight ankle edema has resolved, but the back pain and the inability to sleep continues
Physical: No changes noted
Questions:
- Considering SJ’s race, what class(s) of antihypertensive medications would the nurse anticipate being ordered at this time?
- What signs does SJ have indicating that the patient has chronic hypertension?
- What new teaching will the patient need once a medication has been prescribed?
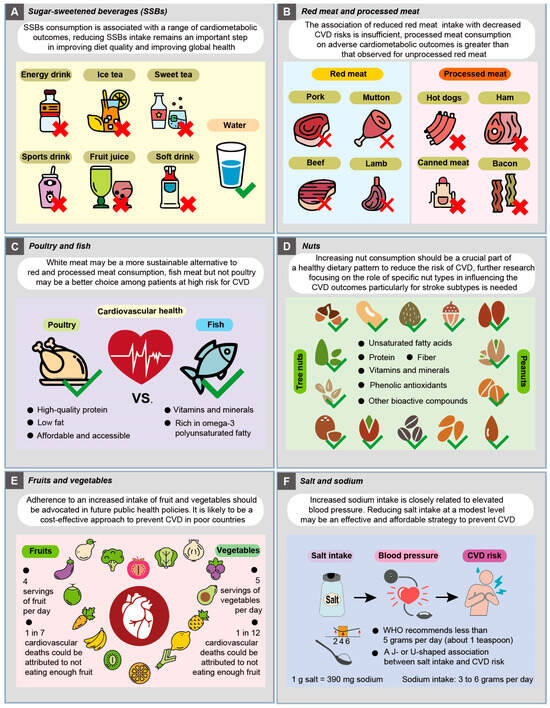
Hyperlipidemia: Antilipemic also call anti-cholesterol medications
Hyperlipidemia
Cholesterol is a fat (also called a lipid) that your body needs to work properly to produce cell membranes, hormones, and Vitamin D (Martin, S. S. 2024). However, too much bad cholesterol can increase the risk of heart disease, stroke, and peripheral vascular disease. The medical term for high blood cholesterol is hyperlipidemia.
There are many types of cholesterol.
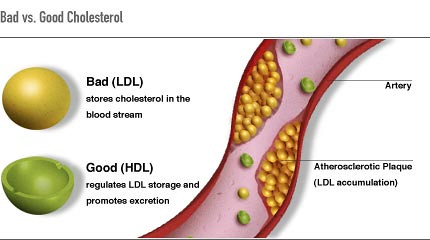
There are many types of cholesterol:
- Total cholesterol: All the cholesterols combined
- High-density lipoprotein (HDL) cholesterol is often called “good” because it promotes excretion. Exercise helps to increase HDL and remove cholesterol from the bloodstream
- Low-density lipoprotein (LDL) cholesterol: Often called “bad” cholesterol because it stores cholesterol in the bloodstream, which contributes to atherosclerosis
The table below identifies normal from abnormal levels of cholesterol:
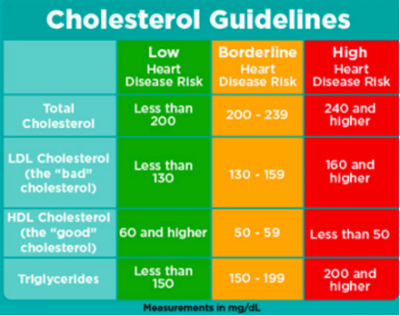
National Cholesterol Education Program Guidelines, 2018
Dietary and other lifestyle changes, including exercise, are the initial approach to lowering cholesterol.
Antilipemic Medications
Antilipemic agents reduce hyperlipidemia, which may lead to additional health problems such as stroke, myocardial infarction, angina, and heart failure. Medications should be used in conjunction with a healthy diet and exercise regime approved by the patient’s healthcare provider.
Class off Antihyperlipidemic medications include:
Statins (Atorvastatin, Simvastatin, and others).
- These drugs decrease the amount of cholesterol made by the liver and are already in the blood, and there is evidence that they may reduce inflammation in the artery walls.
PCSK9 inhibitors (Alirocumab, Evolocumab, and others).
- PCSK9 is a protein found in the liver that regulates cholesterol metabolism. More specifically, it stops the breakdown of LDL, leading to familial hypercholesterolemia. Therefore, the PCSK9 inhibitors decrease cholesterol by clearing LDL cholesterol.
Fibric acid derivatives or fibrates (Gemfibrozil, Fenofibrate, and others).
- “Decrease low-density lipoprotein cholesterol (LDL-C), total cholesterol, triglycerides, and apolipoprotein B and increase high-density lipoprotein cholesterol (HDL-C-good cholesterol) (Matthew, C. T. & Paramvir, S 2023).”
- It must be used with low cholesterol – low-fat diet and exercise.
Bile acid sequestrants or bile acid resins (Cholestyramine, Colesevelam, and others).
- Reduces cholesterol by stopping the production of bile acids, which, if produced, increases cholesterol. It lowers LDL-C. An insoluble complex is formed, and all the medication taken is excreted in the feces and bile acids removed from the enterohepatic circulation (Lent-Schochet, D. & Jialal, I. 2023). Certain medications in this class of drugs can be used by children and adolescents
Nicotinic acid or niacin (Niacin and others).
- This is Vitamin B3 that may boost levels of good HDL cholesterol, modestly lowering bad LDL cholesterol and lower triglycerides. May be prescribed with statins for cholesterol control (Greenwood, B.G., Griffin, R. G., Gopal, A. 2024)
Selective cholesterol absorption inhibitors (Ezetimibe and others).
- It prevents the uptake of cholesterol from the small intestine to the circulatory system by binding to bile acids and preventing the creation of new cholesterol. These medications are formulated as viscous soluble fiber or fiber supplements.
Omega-3 fatty acids and fatty acid esters (Alpha-linolenic acid-ALA and others).
- It lowers triglyceride levels, raises HDL cholesterol, and lowers blood pressure. This synergistic effect decreases the risk of heart disease and stroke.
Adenosine triphosphate-citrate lyase (ACL) inhibitors (Bempedoic acid and others).
- These are a new class of drugs that work by inhibiting the enzyme ACL, which then inhibits the HMG-CoA enzyme. This decreases the formation and use of formerly produced circulating cholesterol. Additionally, these drugs help the body rid itself of some LDL cholesterol.
Examples of widely used Antilipemic include:
- An example of a Statin is Atorvastatin
Example: Atorvastatin
Mechanism of Action: Atorvastatin inhibits HMG-CoA reductase and cholesterol synthesis, which reduces LDL (low-density lipoprotein).
Indication of Use: This medication is used for hyperlipidemia and the prevention of cardiovascular disease.
Nursing Consideration Across the Lifespan: Do not use this medication with patients who have hepatic disease. It is also contraindicated with patients who are pregnant or breastfeeding. Do not give it to patients under 10 years of age. Use caution with geriatric patients due to the increased risk for myopathy.
Adverse/Side Effects: Patients who are pregnant or breastfeeding should not take this medication. A healthcare provider will assess routine liver function for a patient taking atorvastatin. Nausea, diarrhea, dyspepsia, increase in blood glucose, rhabdomyolysis, myalgia, or muscle spasms may be produced by taking this medication. Rhabdomyolysis is when damaged skeletal muscle breaks down rapidly, causing muscle pain and weakness. Some of the muscle breakdown products are harmful to the kidneys and can cause kidney failure. There may be tea-colored urine or an irregular heartbeat with rhabdomyolysis.
Patient Teaching & Education: Patients should take the prescribed medication as directed and avoid consuming grapefruit juice during drug therapy. The medication should be used with dietary modifications. If the patient experiences muscle pain, tenderness, or weakness, these should be reported to the healthcare provider.
2. An example of a Selective Absorption Cholesterol Inhibitor is Ezetimibe
Ezetimibe
Mechanism of Action: Ezetimibe blocks the absorption of cholesterol in the small intestines to reduce LDL.
Indication of Use: This medication is used for the treatment of hyperlipidemia and familial hypercholesterolemia.
Nursing Consideration Across the Lifespan: If medication is combined with HMG-CoA reductase inhibitors, do not give to pregnant or breastfeeding patients.
Adverse/Side Effects: Use caution when ezetimibe is combined with additional medication. Patients may experience arthralgia, rhabdomyolysis, hepatic impairment, dizziness, upper respiratory infections, or diarrhea if they are taking this medication. Minimal side effects were reported with monotherapy.
Patient Teaching & Education: Patients should take the prescribed medication as directed and avoid consuming grapefruit juice during drug therapy. The medication should be used with dietary modifications. If the patient experiences muscle pain, tenderness, or weakness, this should be reported to the healthcare provider.
An example of an antilipemic medication Card
Now, let’s take a closer look at the medication card for atorvastatin.
Medication Card: Antilipemics (Atorvastain (lipitor))
Class: Antilipemic
Prototypes: Atorvastatin (Lipitor)
Mechanism: Atorvastatin inhibits HMG-CoA reductase and cholesterol synthesis, which reduces LDL (low-density lipoprotein)
Therapeutic Effects
- Decreases Lipid levels LDL’s
- Improves blood flow through blood vessels by reducing cholesterol synthesis
Administration
- Administered PO 10-80 mg daily (dose depends on prescribing MD)
- Increasing doses happen every 2-4 weeks until therapeutic lipid blood levels
- Do not stop taking it unless advised by the doctor
- Keep away from children and moisture (avoid bathroom storage)
Indications
- Hyperlipidemia
- Prevention of Cardiac disease
- Prevention of Stroke
- Reduce risk post-revascularization procedures
Contraindications
- People with Hepatic disease
- Pregnant or breastfeeding
- Children under 10 years of age (make sure to check guidelines in your setting)
- Cyclosporine
- Gemfibrozil
- Red yeast rice
Side Effects
- Nausea and diarrhea
- Dyspepsia
- Increased blood glucose
- Rhabdomyolysis- kidney damage resulting, so watch for kidney function
- Myalgia
- Muscle pain and weakness
- Tea colored urine
- Irregular heartbeat
- SAFETY: Report muscle pain, yellow skin, decrease in urine, and abdominal pain to serious complications can arise
Nursing Considerations
- Caution in giving to geriatric patients due to increased risk for myopathy
- Assess routine liver and kidney function tests, and Hb1AC increases possible with statins
- Do not drink or eat grapefruit
Why is there a need for combination therapy?
Monotherapy rarely works to manage hypertension, especially if blood pressure readings are greater than is seen in Stage 1 hypertension. Approximately 70% of patients treated for hypertension need at least two different classes of antihypertensives to effectively treat their hypertension. New data indicates that dual therapy is appropriate for initial therapy. The drugs most commonly used in combination therapy include diuretics and β-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, and ACE inhibitors and calcium antagonists. An anti-lipidemic may also be needed to protect the patient from cardiac disease and even stroke.
Combination therapy enables several perks, including;
- A distinct decrease in blood pressure readings
- A decrease in the side effect profile as lower doses of both medications are used to treat the patient.
- Adherence to the medication plan increases.
- A decrease in cost is noted.
V. Conditions and Disorders Related to Perfusion/Uncontrolled Hypertension
Diseases/Disorders that are associated with Hypertension
Edema
Despite valves within larger veins, some blood will inevitably pool in the lower limbs over a day due to the pull of gravity. Any blood that accumulates in a vein will increase the pressure within it. Increased pressure will promote the flow of fluids out of the capillaries and into the interstitial fluid. The presence of excess tissue fluid around the cells leads to a condition called edema. Here is an image of a patient with pitting edema.

Most people experience daily fluid accumulation in their tissues, especially if they spend much time on their feet (like most health professionals). However, clinical edema goes beyond normal swelling and requires medical treatment. Edema has many potential causes, including hypertension and heart failure, severe protein deficiency, and renal failure. Diuretics such as furosemide are used to treat edema by causing the kidneys to eliminate sodium and water.
Arteriosclerosis
Arteriosclerosis begins with injury to the endothelium of an artery, which may be caused by irritation from high blood glucose, infection, tobacco use, excessive blood lipids, and other factors. Injured artery walls cause inflammation. As inflammation spreads into the artery wall, it weakens and scars it, leaving it stiff. Circulating triglycerides and cholesterol can seep between the damaged lining cells and become trapped within the artery wall, where leukocytes, calcium, and cellular debris join them. Eventually, this plaque buildup can narrow arteries enough to impair blood flow. The term for this condition, atherosclerosis, describes the plaque deposits. See below for an illustration of atherosclerosis.
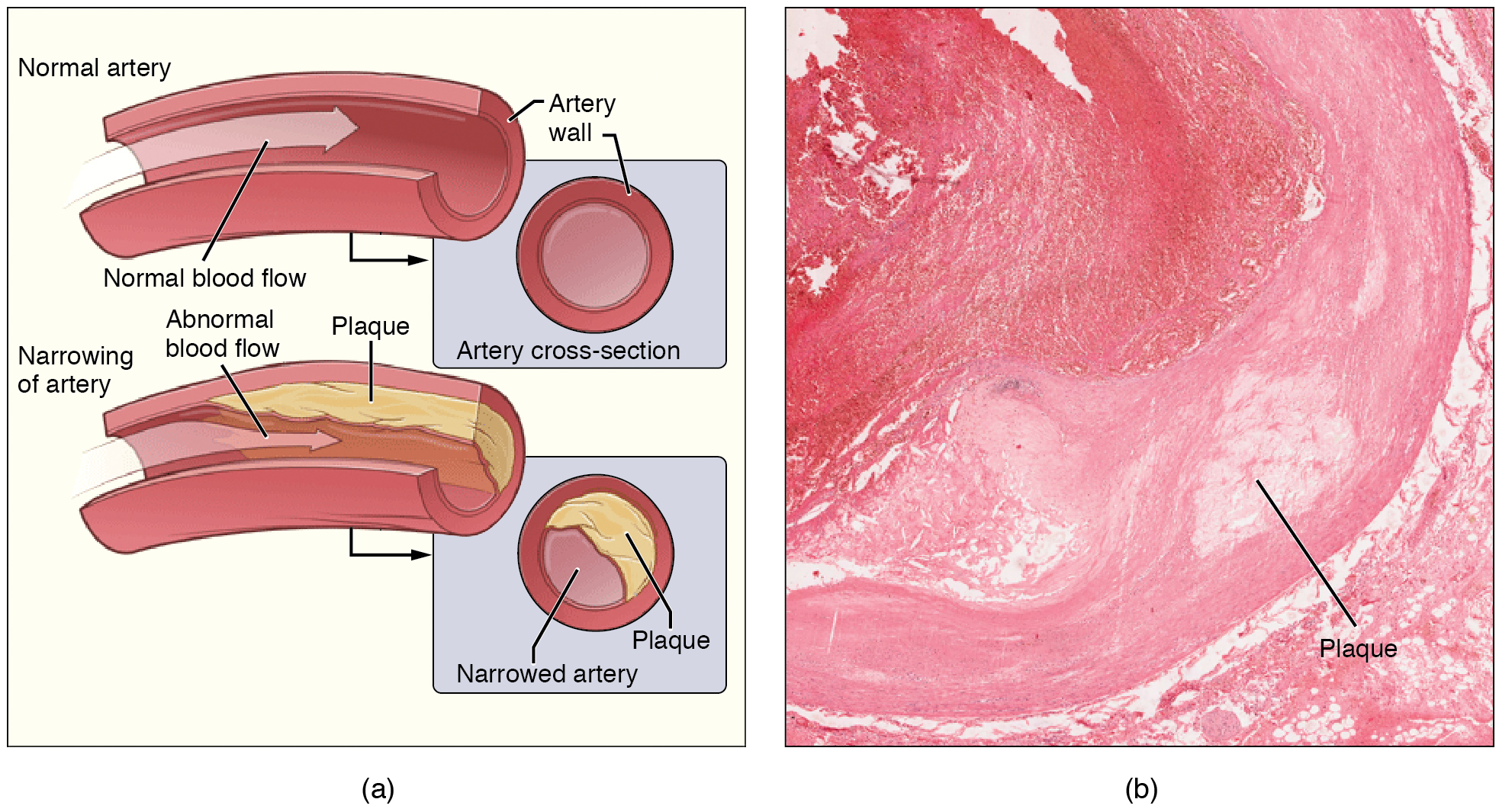 Atherosclerosis
AtherosclerosisSometimes, plaque can rupture, causing microscopic tears in the artery wall that allow blood to leak into the tissue on the other side. When this happens, platelets rush to the site to clot the blood. This clot can further obstruct the artery and—if it occurs in a coronary or cerebral artery—cause a sudden heart attack or stroke. Alternatively, plaque can also break off and travel through the bloodstream as an embolus until it blocks a more distant, smaller artery.
Even without total blockage, narrowed vessels lead to ischemia (reduced blood flow to the tissue region “downstream” of the narrowed vessel). Ischemia can lead to hypoxia (decreased supply of oxygen to the tissues), causing a myocardial infarction or cerebrovascular accident.
The treatment of atherosclerosis includes lifestyle changes, such as weight loss, smoking cessation, regular exercise, and a diet low in sodium and saturated fats. Antilipemic drugs, such as Atorvastatin, are prescribed to reduce cholesterol and help prevent atherosclerosis.
Coronary Artery Disease
Coronary artery disease is the leading cause of death worldwide. It occurs when atherosclerosis within the walls of the coronary arteries obstructs blood flow. As the coronary blood vessels become blocked with plaque, the flow of blood to the tissues is restricted, causing the cardiac cells to receive insufficient amounts of oxygen, which can cause pain called angina. Figure 6.3 (see below) shows the blockage of coronary arteries highlighted by the injection of dye. Some individuals with coronary artery disease report pain radiating from the chest called angina, but others, especially women, may remain asymptomatic or have alternative symptoms of neck, jaw, shoulder, upper back, or abdominal pain. If untreated, coronary artery disease can lead to myocardial infarction (heart attack). Risk factors include smoking, family history, hypertension, obesity, diabetes, lack of exercise, stress, and hyperlipidemia. Treatments may include medication, changes to diet and exercise, a coronary angioplasty with a balloon catheter, insertion of a stent, or a coronary bypass procedure.
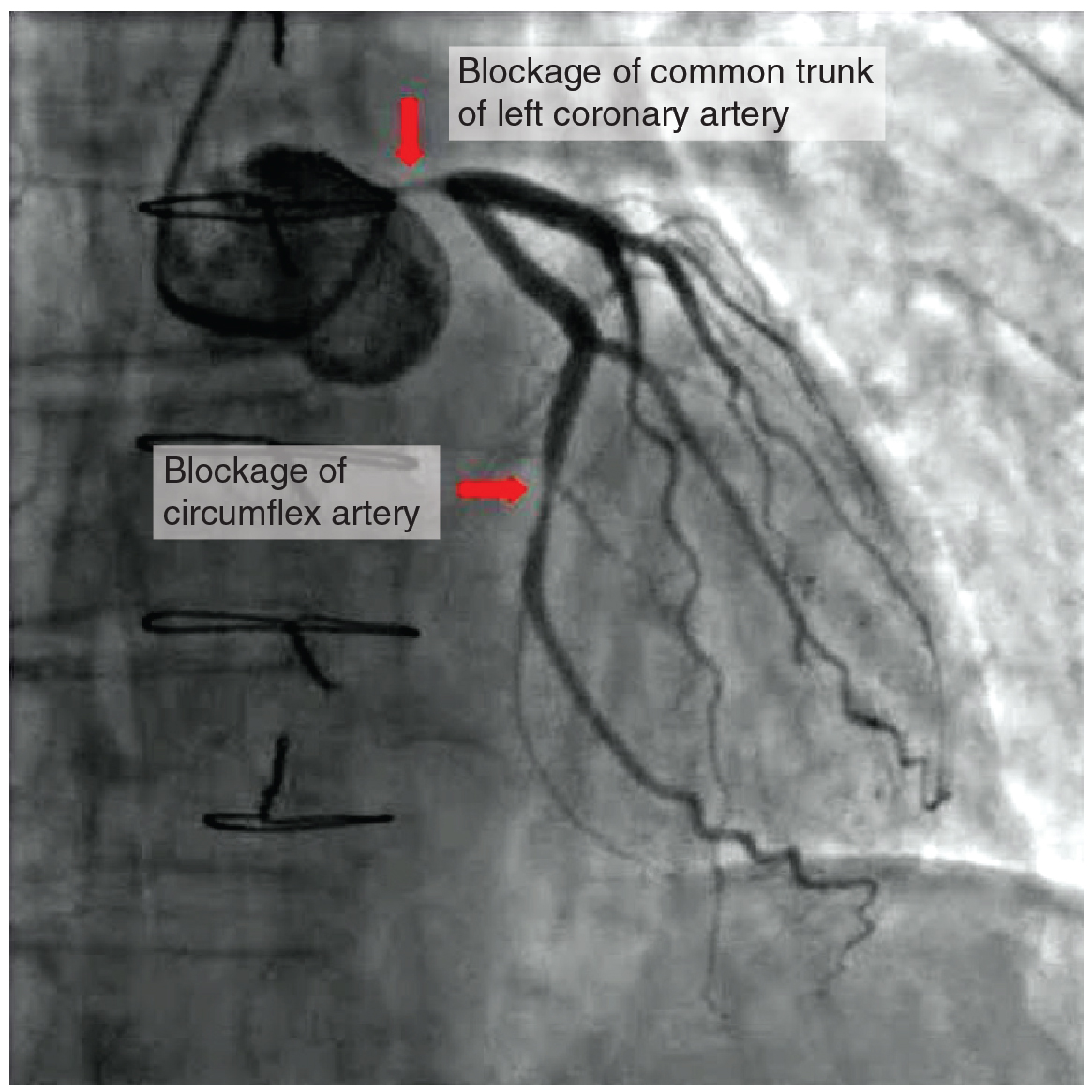
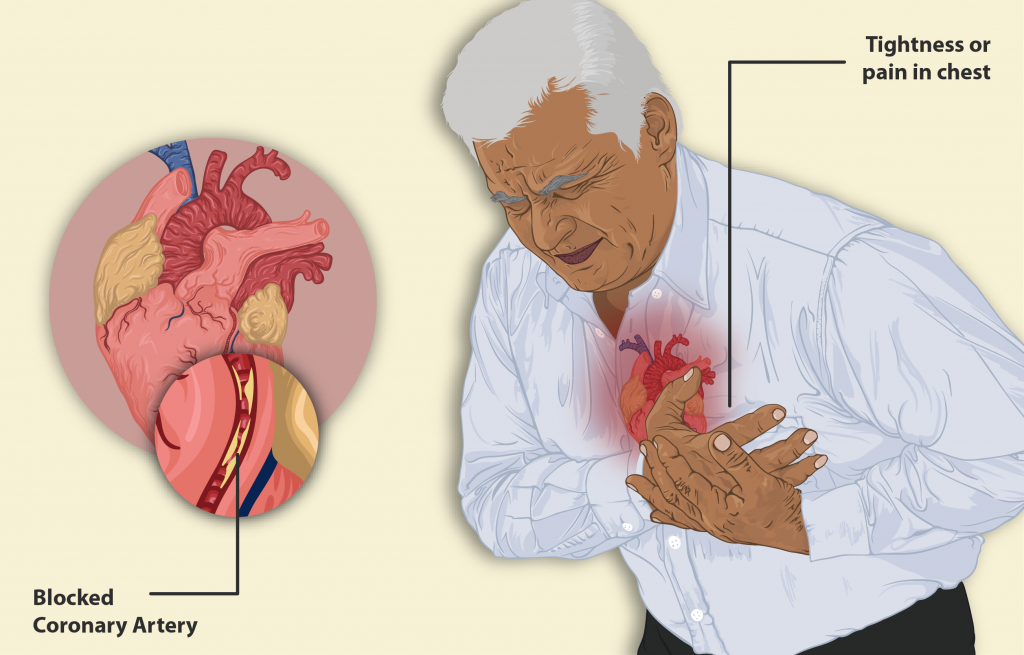
Myocardial Infarction
Myocardial infarction (MI) is the medical term for what is commonly referred to as a “heart attack.” It results from a lack of blood flow and oxygen to a region of the heart, resulting in the death of the cardiac muscle cells. An MI often occurs when the buildup of atherosclerotic plaque blocks a coronary artery and becomes a thrombus or when a portion of an unstable atherosclerotic plaque travels through the coronary arterial system and lodges in one of the smaller vessels.
In the case of acute MI, there is often sudden pain beneath the sternum (retrosternal pain) called angina, often radiating down the left arm in male patients but not as commonly in female patients. In addition, patients typically present with difficulty breathing and shortness of breath (dyspnea), irregular heartbeat (palpitations), nausea and vomiting, sweating (diaphoresis), anxiety, and fainting (syncope), although not all of these symptoms may be present. Many of the symptoms are shared with other medical conditions, including anxiety attacks and simple indigestion, so accurate diagnosis is critical for survival.
An MI can be confirmed by examining the patient’s ECG, which frequently reveals ST and Q component alterations. Immediate MI treatments are required, including administering supplemental oxygen, aspirin, and nitroglycerin. Longer-term treatments may include injections of thrombolytic agents, such as the tissue plasminogen activator, also known as tPA, that dissolve the clot; the anticoagulant heparin; a balloon angioplasty with stents to open blocked vessels; or bypass surgery to allow blood to pass around the site of the blockage. Please note that drugs such as tPA are used in emergency and intensive care units.
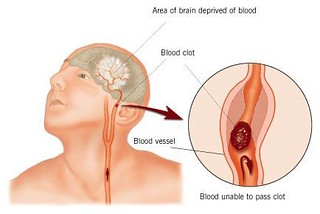
Cerebrovascular Accident (CVA)
The internal carotid and vertebral arteries are the two primary blood suppliers to the human brain. Given the brain’s central role and vital importance to life, the blood supply to this organ must remain uninterrupted. However, blood flow may become obstructed due to atherosclerosis or an embolus that has traveled from elsewhere in the blood. For example, an arrhythmia called atrial fibrillation can cause clots to form in the heart and then move to the brain. When blood flow is interrupted, even for just a few seconds, a transient ischemic attack (TIA), or mini-stroke, may occur, resulting in loss of consciousness or temporary loss of neurological function. Loss of blood flow for longer periods produces irreversible brain damage or a stroke, also called a cerebrovascular accident (CVA). There are two types of cerebrovascular accidents: ischemia and hemorrhagic. Ischemic strokes are caused by atherosclerosis or a blood clot that blocks blood flow to the brain. Eighty percent of strokes are ischemic. Hemorrhagic strokes are caused by a blood vessel that ruptures and bleeds into the brain. Risk factors for a stroke include smoking, high blood pressure, and cardiac arrhythmias. Treatment of a stroke depends on the cause. Ischemic strokes are treated with thrombolytic medication such as tPA to dissolve the clot, whereas hemorrhagic strokes often require surgery to stop the bleeding.
A male 65-year-old patient has the following medications ordered: metoprolol succinate 100 mg daily, lisinopril 5 mg daily, verapamil ER 100 mg daily, and hydrochlorothiazide 25 mg daily. He has a history of hyperlipidemia, hypertension, and coronary artery disease. The patient asks the nurse, “Why do I have to take so many medications?”
- What is the class and mechanism of action of each of these medications?
- What is the nurse’s best response to the patient’s question?
Clinical Learning Exercise:
Create an illustration or a concept map of how various classes of antihypertensive medications and anti-lipidemic act on various cells/organs of the body that enhance perfusion.
References:
Management of Hypertension With Non-pharmacological Interventions: A Narrative Review
P, Okeke M, Guntuku S, Lingamsetty SSP, Slonovschi E. Management of Hypertension With Non-pharmacological Interventions: A Narrative Review. Cureus. 2023 Aug 6;15(8):e43022. doi: 10.7759/cureus.43022. PMID: 37674940; PMCID: PMC10478605.
https://my.clevelandclinic.org/health/treatments/antihyperlipidemic
Chen W, Zhang S, Hu X, Chen F, Li D. A Review of Healthy Dietary Choices for Cardiovascular Disease: From Individual Nutrients and Foods to Dietary Patterns. Nutrients. 2023; 15(23):4898. https://doi.org/10.3390/nu15234898
The Scoop on Statins: What Do You Need to Know? https://millionhearts.hhs.gov/learn-prevent/scoop-on-statins.html#:~:text=Statins%20are%20a%20class%20of,is%20already%20in%20the%20blood.
Hajar R. (2019). PCSK 9 Inhibitors: A Short History and a New Era of Lipid-lowering Therapy. Heart views : the official journal of the Gulf Heart Association, 20(2), 74–75. https://doi.org/10.4103/HEARTVIEWS.HEARTVIEWS_59_19
Mathew CT, Singh P. Fibric Acid Antilipemic Agents. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538508/
Lent-Schochet D, Jialal I. Antilipemic Agent Bile Acid Sequestrants. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549906/
Niacin (Vitamin B3)Medically Reviewed by Jabeen Begum, MD on May 22, 2024 Written by Brigid Galloway Greenwood, R. Morgan Griffin, Amy Gopal https://www.webmd.com/diet/supplement-guide-niacin
Cholesterol absorption inhibitor https://en.wikipedia.org/wiki/Cholesterol_absorption_inhibitor
Omega-3 Fatty Acids: https://my.clevelandclinic.org/health/articles/17290-omega-3-fatty-acids
How Do ACL Inhibitors Work? Dr. Sruthi M., MBBS https://www.rxlist.com/how_do_acl_inhibitors_work/drug-class.htm#:~:text=ACL%20inhibitors%20are%20a%20new,biosynthesis%20pathway%20in%20the%20liver.
Media Attributions
- Renin-Angiotensin
- Complications_of_hypertension_whitebackground


