6 Perfusion: Coagulation Disorders and Anticoagulants Medications
This chapter covers the concepts of perfusion, focusing on coagulation and its pharmacologic principles. These are essential concepts that professional nurses must apply in various healthcare settings. Understanding the pathophysiology of coagulation disorders is crucial for the pharmacologic management and nursing care of affected patients.
Learning Objectives
- Understand the etiology, pathophysiology, and clinical manifestations of hemostasis and coagulation.
- Discuss non-pharmacologic measures to control clotting disorders and interventions to increase therapeutic effects.
- Explain the mechanism of action, indications for use, adverse effects, and implications of the nursing process for anticoagulants, antiplatelet, direct thrombin inhibitors, and thrombolytic agents.
- Compare heparins and warfarin in terms of indications of use, onset, and duration of action, route of administration, and laboratory tests used to monitor effects.
- Describe systemic hemostatic agents for treating overdoses of anticoagulant and thrombolytic medications.
I. Perfusion Overview
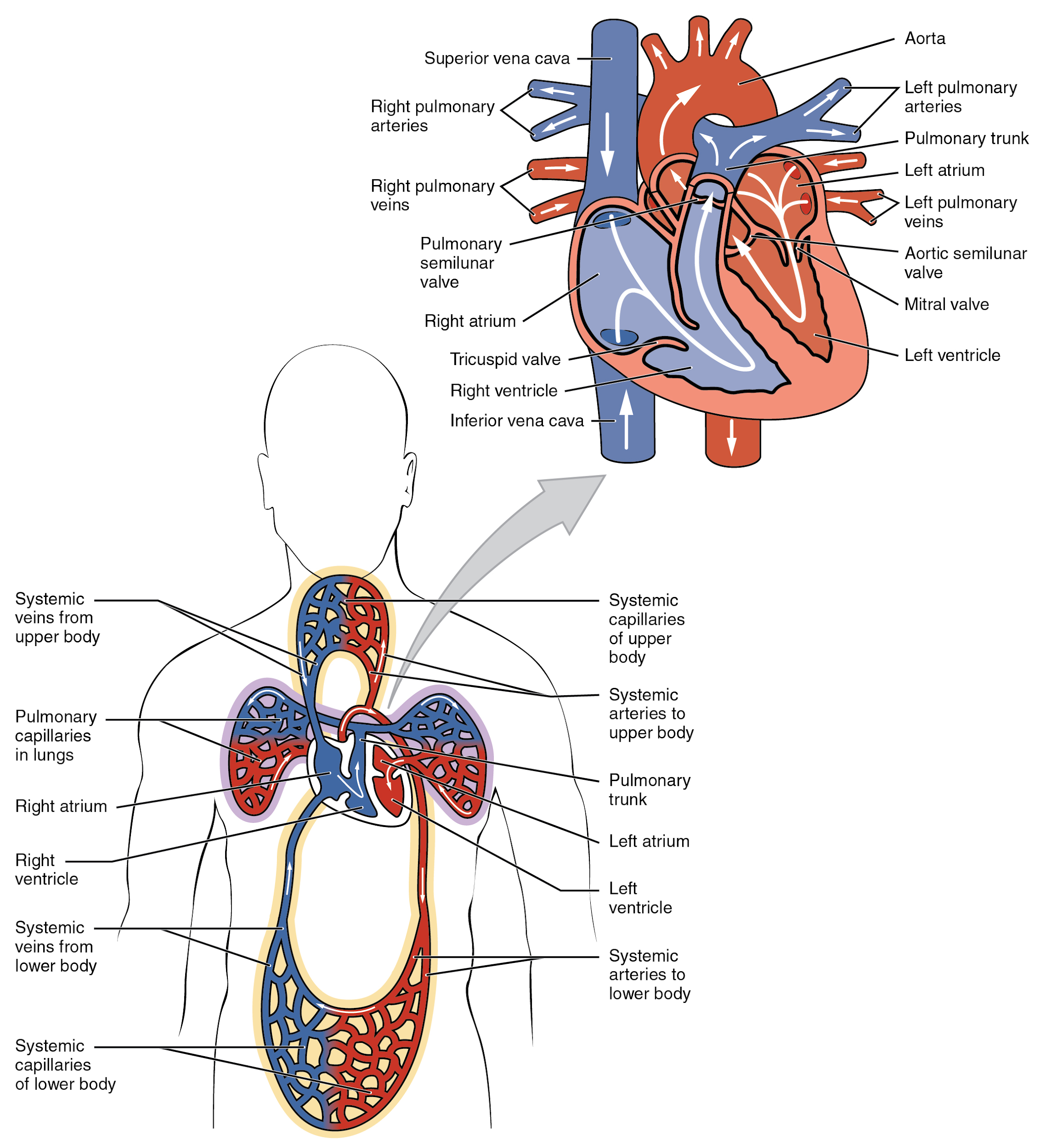
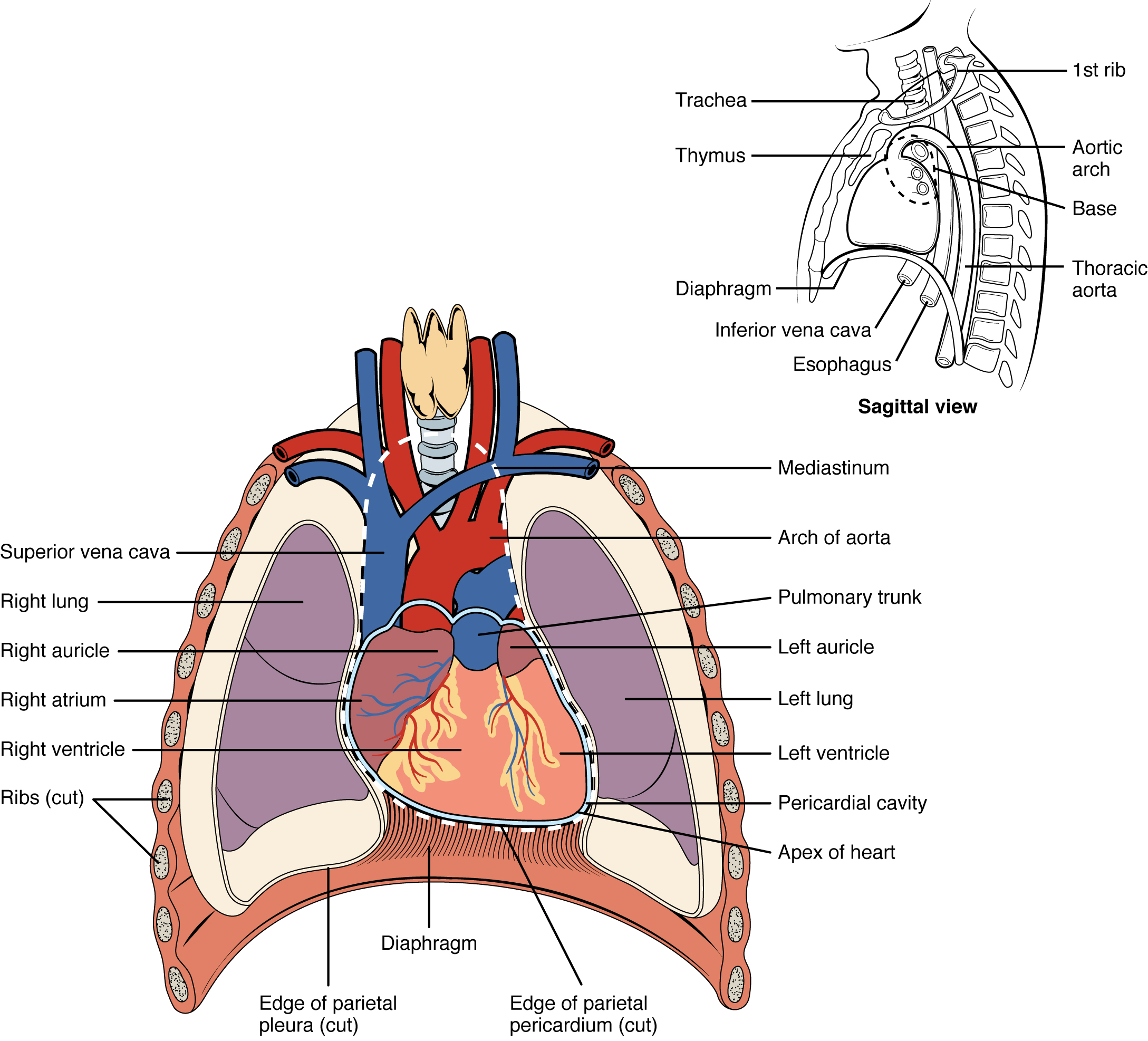
Perfusion is the heart’s ability to circulate oxygen and nutrients throughout the body to support cellular functions. It operates cyclically, removing cellular wastes and by-products as cells receive oxygen and nutrients. This chapter reviews the body systems that maintain adequate perfusion, including the cardiovascular and renal systems, to ensure survival.
The Heart
Did you know that the average adult human heart contracts approximately 108,000 times a day, over 39 million times a year, and nearly 3 billion times over a 75-year lifespan? Each heartbeat ejects about 70 mL of blood, producing 5.25 liters per minute and around 14,000 liters daily. This equates to over 2.6 million gallons of blood annually through approximately 60,000 miles of vessels in the adult body. No wonder the heart is the body’s most important muscle! This chapter reviews key concepts and disorders related to the heart and cardiovascular system, followed by standard medication classes. Understanding these medications is crucial for nurses to provide safe and effective patient care.
Main Function of the Heart
Oxygenating and Nourishing Organs and Tissues
- The heart circulates oxygenated blood, nutrients, and hormones to organs and tissues, enabling essential processes that sustain life. Without proper blood flow, cells risk oxygen deprivation, impairment, and death.
Removing Waste Products from Organs and Tissues
- The heart also circulates deoxygenated blood and metabolic wastes away from the body for excretion. This allows blood to be re-oxygenated and the cycle to continue.
II. Hemostasis and Coagulation: Etiology, Pathophysiology, and Clinical Manifications
Etiology
Hemostasis is the physiological process that stops bleeding at the site of an injury while maintaining normal blood flow elsewhere in the circulation.
Coagulation is a key component of hemostasis, involving the transformation of blood from a liquid to a solid state to form a clot. The etiology of disorders related to hemostasis and coagulation can be broadly categorized into:
- Genetic Factors:
- Hemophilia: An inherited disorder where specific clotting factors (Factor VIII in hemophilia A and Factor IX in hemophilia B) are deficient or defective.
- Von Willebrand Disease: A genetic disorder caused by missing or defective von Willebrand factor (vWF), a clotting protein.
- Acquired Factors:
- Vitamin K Deficiency: Essential for the synthesis of clotting factors II, VII, IX, and X.
- Liver Disease: The liver produces most of the clotting factors, and liver dysfunction can impair clotting.
- Medications: Anticoagulants (e.g., warfarin, heparin) and antiplatelet drugs (e.g., aspirin, clopidogrel) can alter normal coagulation processes.
- Autoimmune Disorders: Conditions like antiphospholipid syndrome can lead to abnormal clot formation.
- Environmental Factors:
- Trauma or Surgery: Physical injury or surgical procedures can disrupt normal hemostasis.
- Infections: Certain infections can induce disseminated intravascular coagulation (DIC), a severe condition characterized by widespread clotting and bleeding.
Pathophysiology
Hemostasis and coagulation involve a complex interplay of vascular, platelet, and plasma components:
- Vascular Phase:
- Vasoconstriction (vascular spasm): Immediately after a vascular injury, blood vessels constrict to reduce blood flow to the damaged area.
- Platelet Phase (Formation of the Platelet Plug):
- Platelet Adhesion: Platelets adhere to the exposed collagen fibers at the injury site.
- Platelet Activation: Adhered platelets become activated and release granules containing ADP, thromboxane A2, and other factors that attract additional platelets.
- Platelet Aggregation: Activated platelets aggregate to form a temporary “platelet plug.”
3. Coagulation Phase:
The more sophisticated and durable repairs are called coagulation, or the formation of a blood clot. The process is sometimes characterized as a cascade because one event prompts the next, as in a multi-level waterfall. The result is the production of a gelatinous but robust clot made of a mesh of fibrin in which platelets and blood cells are trapped. The figure below summarizes the three steps of hemostasis when an injury to a blood vessel occurs. First, a vascular spasm constricts the flow of blood—next, a platelet plug forms to temporarily seal small openings in the vessel. Coagulation then enables the repair of the vessel wall once the leakage of blood has stopped. The synthesis of fibrin in blood clots involves either an intrinsic or extrinsic pathway, both of which lead to a common pathway creating a clot.
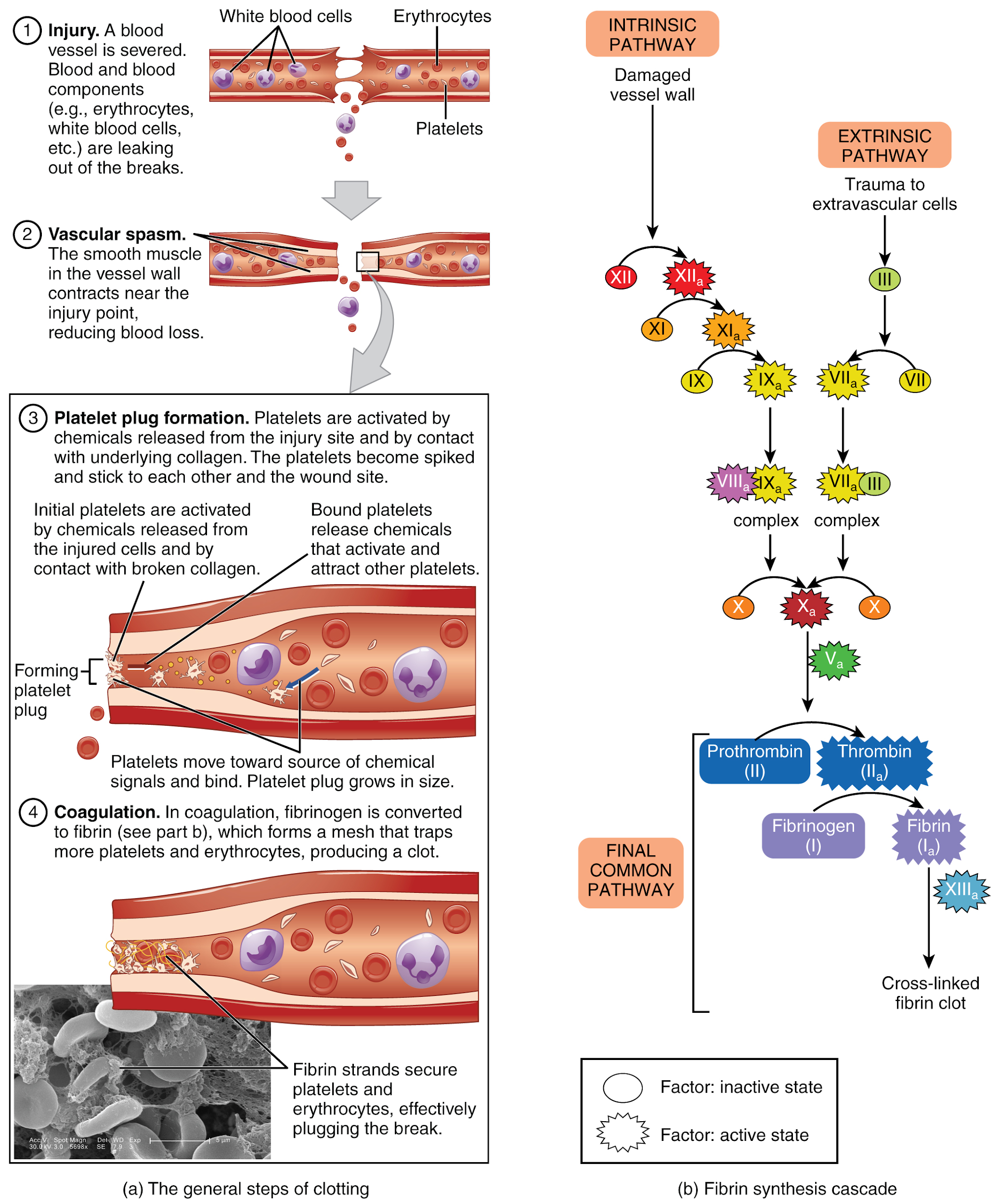
Extrinsic Pathway: The quicker-responding and more direct extrinsic pathway (also known as the tissue factor pathway) begins when damage occurs to the surrounding tissues, such as in a traumatic injury. The events in the extrinsic pathway are completed in seconds.
Intrinsic Pathway: The intrinsic pathway is longer and more complex. In this case, the factors involved are intrinsic to (present within) the bloodstream. The pathway can be prompted by tissue damage or internal factors such as arterial disease. The events in the intrinsic pathway are completed in a few minutes.
Common Pathway: Both the intrinsic and extrinsic pathways lead to the common pathway, where fibrin is produced to seal off the vessel. Once Factor X has been activated by either the intrinsic or extrinsic pathway, Factor II, the inactive enzyme prothrombin, is converted into the active enzyme thrombin. Then, thrombin converts Factor I, the soluble fibrinogen, into the insoluble fibrin protein strands. Factor XIII then stabilizes the fibrin clot.
Fibrinolysis: Contractile proteins within the platelets act on the stabilized clot. As these proteins contract, they pull on the fibrin threads, bringing the edges of the clot more tightly together, somewhat like we do when tightening loose shoelaces. This process also wrings out of the clot a small amount of fluid called serum, which is blood plasma without clotting factors.
The clot must eventually be removed to restore normal blood flow as the vessel heals. Fibrinolysis is the gradual degradation of the clot. Again, a fairly complicated series of reactions involves Factor XII and protein-catabolizing enzymes. During this process, the inactive protein plasminogen is converted into the active plasmin, which gradually breaks down the fibrin of the clot. Additionally, bradykinin, a vasodilator, is released, reversing the effects of the serotonin and prostaglandins from the platelets. This allows the smooth muscle in the walls of the vessels to relax and helps to restore circulation.
Plasma Anticoagulants: An anticoagulant is any substance that opposes coagulation. Several circulating plasma anticoagulants play a role in limiting the coagulation process to the region of injury and restoring a normal, clot-free condition of blood. For instance, antithrombin inactivates Factor X and opposes the conversion of prothrombin (Factor II) to thrombin in the common pathway. Basophils release heparin, a short-acting anticoagulant that also opposes prothrombin. A pharmaceutical form of heparin is often administered therapeutically to prevent or treat blood clots.
A thrombus is an aggregation of platelets, erythrocytes, and WBCs typically trapped within a mass of fibrin strands. While clot formation is normal following the hemostatic mechanism just described, thrombi can form within an intact or only slightly damaged blood vessel. In a large vessel, a thrombus will adhere to the vessel wall and decrease blood flow. In a small vessel, it may block blood flow completely and is termed an occlusive thrombus.
Several medications impact the coagulation cascade. For example, aspirin (acetylsalicylic acid) is very effective at inhibiting the aggregation of platelets. Patients at risk for cardiovascular disease often take a low dose of aspirin daily as a preventive measure. It is also routinely administered during a heart attack or stroke to reduce platelet plug formation.
Another class of drugs known as thrombolytic agents are used to dissolve an abnormal clot. If a thrombolytic agent is administered to a patient within a few hours following a thrombotic stroke or myocardial infarction, the patient’s prognosis improves significantly. Tissue plasminogen activator (TPA) is an example of a medication released naturally by endothelial cells but is also used in clinical medicine to break down a clot.
- Clot Retraction and Repair:
- The clot contracts to reduce its size and pull the wound’s edges together, facilitating tissue repair.
- Fibrinolysis:
- Once the vessel is healed, the clot is dissolved by plasmin, restoring normal blood flow.
Medications
Several medications, including anticoagulants, antiplatelet, and thrombolytics, and their associated reversal agents, affect blood coagulation.
Anticoagulants prevent clot formation by inhibiting certain types of clotting factors. Anticoagulants include the following drug classes: heparins or unfractionated heparin and low molecular weight heparin (LMWH), warfarin (Coumadin), selective factor Xa inhibitors (rivaroxaban), and direct thrombin inhibitors (dabigatran). Antiplatelet include aspirin and other aggregation inhibitors such as clopidogrel, and thrombolytics include alteplase (tPA). All these medications are included on the List of High Alert Medications (HAMs) by the Institute for Safe Medication Practices (ISMP) and require special safeguards to reduce the risk of errors or adverse effects.
The most common anticoagulant errors in acute hospital settings are administration mistakes, including incorrect dosage calculations and infusion rates. The Health Research and Educational Trust focuses on reducing harm related to HAMs by 50% and recommends the following interventions to achieve this goal:
- Educate staff based on evidence and best practices.
- Use standardized order sets and protocols.
- Perform medication reconciliation at all transitions.
Specific interventions regarding anticoagulant therapy include standardizing protocols for withholding and restarting warfarin perioperatively, including pharmacists on rounds to provide decision support for staff administering HAMs and reduce prescribing errors, pharmacist monitoring of anticoagulants, and pharmacist notification when rescue medications are given.
According to the Institute for Safe Medication Practices (ISMP) 2016 Annual Report, there is also a high risk of acute injuries for patients taking anticoagulants outside the hospital setting. Anticoagulants are commonly used by the elderly to reduce the risk of ischemic stroke, with an estimated 3.8 million people taking oral anticoagulants in 2016. CDC data show that adverse effects of oral anticoagulants account for more emergency department visits than any other class of drugs. Adverse effects range from gastrointestinal bleeding to cerebral hemorrhages, resulting in over 3,000 deaths in 2016.
Since 1954, warfarin has been a standard but hazardous treatment for preventing blood clots. Warfarin requires close laboratory monitoring and individual dose adjustments based on PT and INR lab results. When the pharmaceutical industry began marketing modern replacements for warfarin, including dabigatran (Pradaxa), rivaroxaban (Xarelto), and apixaban (Eliquis), they designed them to be easier to use than warfarin because no laboratory monitoring was required, but not necessarily safer. Nurses must provide thorough patient and caregiver education for prescribed anticoagulants at home.
Anticoagulants
| Prototype-generic | Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|
| enoxaparin | Use with caution in patients with kidney disease. If used for a patient undergoing neuraxial anesthesia or a spinal puncture, monitor frequently for neurological impairment. If neurological compromise is noted, urgent treatment is necessary. | Prevention or treatment of DVT or PE | Bleeding Risk of hemorrhage
Thrombocytopenia, HIT, or HITT |
| heparin |
Injection (subq) or IV Carefully examine all heparin products to confirm the correct choice before administration. Closely monitor aPTT levels in IV therapy to ensure they are within the therapeutic range. Protamine sulfate is the reversal agent. |
Prevent or treat clots | High risk of bleeding Risk of gastrointestinal or cerebral hemorrhage, especially in elderly
Risk of Heparin-Induced Thrombocytopenia (HIT) and Heparin-Induced Thrombocytopenia and Thrombosis (HITT) |
| warfarin | Oral route
Vitamin K is the antidote Monitor INR results before administering medication Use with caution in patients with liver disease |
Prevent DVT or PE | Bleeding Hemorrhage |
Critical Thinking Activity
A patient who was treated in the hospital for DVT in his left leg has been prescribed warfarin.
1. The patient asks, “Will the warfarin dissolve the clot in my leg?” What is the nurse’s best response?
The nurse plans to assess the patient’s lab work before administering the warfarin.
2. What blood test(s) are important to monitor for patients taking warfarin, and what is the therapeutic range?
The nurse knows that the patient must monitor his diet when taking warfarin.
3. What dietary instructions should be provided to the patient?
The nurse plans to provide patient education regarding this newly prescribed medication.
4. Outline the topics to cover with this high-risk medication.
5. What is the reversal agent for warfarin?
Antiplatelet
Acetylsalicylic acid (aspirin) and clopidogrel (Plavix) are antiplatelet medications.
Chewable aspirin is used during an active myocardial infarction (MI) (heart attack) due to its rapid absorption.
Mechanism of Action
Aspirin inhibits platelet activation and aggregation.
Indications for Use
Aspirin is indicated to reduce the rate of myocardial infarction (MI) and stroke in patients with established peripheral arterial disease or a history of recent MI or stroke. It is also indicated to reduce the rate of MI and stroke in patients with ST-elevation and non-ST-segment elevation ACS.
Nursing Considerations Across the Lifespan
It is important to remember that the effects of these medications last the life of the platelet (7-10 days), so aspirin will need to be withheld for several days before surgery or certain procedures to prevent excessive bleeding. In elderly patients, there is an increased risk of bleeding events with concurrent use of clopidogrel plus aspirin. Aspirin is contraindicated in children under the age of 12 with flu-like symptoms due to the risk of Reye’s syndrome.
Overdose is irreversible.
Clopidogrel is metabolized to its active metabolite by CYP2C19. Concomitant use of drugs that inhibit the activity of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition.
Adverse/Side Effects
Increased risk of bleeding.
Black Box Warning: Reduced effectiveness for patients referred to as “CYP2C19 poor metabolizers.”
Patient Teaching & Education
Patients should report tinnitus, unusual bleeding of the gums, bruising, or blood in the stool to the healthcare provider immediately. To prevent gastric irritation, patients should avoid alcohol and NSAIDs while receiving antiplatelet therapy.
Now, let’s take a closer look at the medication grid for acetylsalicylic acid and clopidogrel in the Table below.
Acetylsalicylic Acid and Clopidogrel Medication Grid
| Class/Subclass | Prototype-generic | Administration Considerations | Therapeutic Effects | Adverse/Side effects |
|---|---|---|---|---|
| Antiplatelet | acetylsalicylic acid (Aspirin) | Administer with food to reduce risk of GI upset and bleeding.
Monitor for bleeding Effects last for 7-10 days |
Prevent MI or stroke | bleeding, GI upset, tinnitus, hematoma |
Thrombolytics
Alteplase (tPA) is a thrombolytic used to break up clots. Its short half-life of 5 minutes allows it to open a clogged artery rapidly. It is often given with heparin to prevent re-occlusion of the affected blood vessel. A smaller dosage form is also used to flush clogged IVs or arterial lines.
Mechanism of Action
Alteplase binds to fibrin in a thrombus and converts the entrapped plasminogen to plasmin, thus breaking down the clot.
Indications for Use
Alteplase is indicated for the acute treatment of myocardial infarction (MI), stroke, or massive pulmonary embolism (PE). It also clears central lines, such as a peripherally inserted central line catheter (PICC).
Nursing Considerations Across the Lifespan
The drug is contraindicated in situations in which the risk of significant bleeding is greater than the potential benefit, such as:
- Active internal or intracranial bleeding
- History of a recent stroke
- Recent (within three months) intracranial or intraspinal surgery or serious head trauma
- Presence of intracranial conditions that may increase the risk of bleeding (e.g., some neoplasms, arteriovenous malformations, or aneurysms)
- Current severe uncontrolled hypertension
Significant post-administration monitoring is performed due to the risk of life-threatening bleeding.
Adverse/Side Effects
This drug can cause significant, sometimes fatal, internal or external bleeding, especially at arterial and venous puncture sites. Avoid intramuscular injections and perform venipunctures carefully and only as required. It can increase the risk of thrombo-embolic events in patients with high likelihood of left heart thrombus, such as patients with atrial fibrillation.
Patient Teaching & Education
Patients must institute bleeding precautions to prevent complications of therapy.
Now, let’s take a closer look at the medication grid for alteplase in the table below.
| Class/Subclass | Prototype-generic | Administration Considerations | Therapeutic Effects | Adverse/Side Effects |
|---|---|---|---|---|
| Thrombolytic | alteplase (tPA) | Contraindicated in many conditions where the risk of bleeding outweighs the potential benefit | Break down a life-threatening clot in MI, stroke, or massive PE | Risk of severe bleeding that can be fatal |
Clinical Manifestations
The clinical manifestations of hemostasis and coagulation disorders can vary widely depending on whether there is excessive bleeding or clotting:
- Bleeding Disorders:
- Easy Bruising and Hematomas: Frequent and large bruises from minor injuries.
- Prolonged Bleeding: Extended bleeding from cuts, surgical sites, or after dental procedures.
- Spontaneous Bleeding: Nosebleeds (epistaxis), gum bleeding, or excessive menstrual bleeding (menorrhagia).
- Joint and Muscle Bleeding: In hemophilia, bleeding into joints (hemarthrosis) and muscles is common.
- Clotting Disorders:
- Deep Vein Thrombosis (DVT): Pain, swelling, and redness in the leg due to clot formation in the deep veins.
- Pulmonary Embolism (PE): Sudden chest pain, shortness of breath, and coughing up blood due to a clot traveling to the lungs.
- Stroke: Sudden neurological deficits caused by a clot obstructing blood flow to the brain.
- Myocardial Infarction (Heart Attack): Chest pain, shortness of breath, and other symptoms resulting from a clot blocking a coronary artery.
Understanding the etiology, pathophysiology, and clinical manifestations of hemostasis and coagulation is crucial for effectively diagnosing and managing these conditions, ensuring appropriate therapeutic interventions to maintain hemostatic balance.
Attributions:
This chapter is partly adapted from:
-
"Position of the Heart in the Thorax" by OpenStax College is licensed under CC BY 4.0.Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"Dual System of the Human Blood Circulation" by OpenStax Collegeis licensed under CC By 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction. ↵
-
"Surface Anatomy of the Heart" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-1-heart-anatomy↵
-
"2018 Conduction System of the Heart" by OpenStax Collegeis licensed under CC BY 4.0 Access it for free at https://openstax.org/books/anatomy-and-physiology/pages/19-2-cardiac-muscle-and-electrical-activity ↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"Electrocardiogram Depolarization.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-2-cardiac-muscle-and-electrical-activity↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"2031 Factors in Cardiac Output.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"2032 Automatic Innervation.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"2036 Summary of Factors in Cardiac Output.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/19-4-cardiac-physiology↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"Combinpedal.jpg" by James Heilman, MDis licensed under CC BY-SA 3.0↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"2626 Renin Aldosterone Angiotensin.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/25-4-microscopic-anatomy-of-the-kidney ↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction. ↵
-
McCuistion, L., Vuljoin-DiMaggio, K., Winton, M, & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 443-454. Elsevier. ↵
-
"2612 Blood Flow in the Kidneys.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney↵
-
"Figure 41 03 04.jpg" by CNX OpenStaxis licensed under CC BY 4.0↵
-
McCuistion, L., Vuljoin-DiMaggio, K., Winton, M, & Yeager, J. (2018). Pharmacology: A patient-centered nursing process approach. pp. 443-454. Elsevier. ↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
"1909 Blood Clotting.jpg" by OpenStax Collegeis licensed under CC BY 4.0 Access for free at https://openstax.org/books/anatomy-and-physiology/pages/18-5-hemostasis↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
This work is a derivative of Anatomy and Physiologyby OpenStax licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction↵
-
Forciea, B. (2018, April 26). Structure of Arteries and Veins V2. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/HZAeua5JbrU↵
-
Forciea, B. (2016, September 14). Muscle Contraction Physiology. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/TB7TypeksGk↵
-
Forciea, B. (2017, April 26). Fluids and Electrolytes Potassium. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/SNAiGaaYkvs↵
-
Forciea, B. (2017, April 24). Fluids and Electrolytes Sodium. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/ar-WrfC7SJs↵
-
Forciea, B. (2015, May 20). Anatomy of the Heart (v2.0). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/d8RSvcc8koo↵
-
Forciea, B. (2015, May 19). Anatomy and Physiology: The Blood. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/bjfcOSoDSzg↵
-
Forciea, B. (2015, May 13). Urinary System Anatomy (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/2Wd45Zmq_Ck↵
-
Forciea, B. (2015, May 13). Renin-Angiotensin System for Anatomy and Physiology (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/iin4lbAKv7Q↵
-
Forciea, B. (2015, May 12). Introduction to the Electrocardiogram (ECG) V2.0. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/mAN0GK7O9yU↵
- Forciea, B. (2015, May 12). Circulatory System