10 Oxygenation: Asthma and Respiratory Drugs
This chapter covers the vital concept of oxygenation, a cornerstone of respiratory physiology and nursing practice. Oxygenation is crucial for maintaining life and supporting cellular function. Nurses must possess a thorough understanding of oxygenation, as it underpins many aspects of patient care and clinical decision-making. From assessing respiratory function to administering oxygen therapy and other respiratory medications, the principles of oxygenation are integral to daily nursing activities. A comprehensive grasp of this concept enables nurses to effectively provide patient care utilizing the nursing process. In this chapter, we will explore the mechanisms of oxygenation and respiratory medications and the critical role nurses play in managing and optimizing oxygenation in diverse healthcare settings.
Learning Objectives
- Understand the etiology, pathophysiology and clinical manifestations of asthma, and other bronchoconstricting disorders.
- Discuss the mechanism of action, indications for use, adverse effects, and nursing process implications for adrenergic, anticholinergic, xanthines, and ant-inflammatory agents.
- Explain the rationales and associated nursing responsibilities for the use of bronchodilators and other anti-inflammatory agents in selected patient populations or purposes.
I. Overview of the Respiratory System.
Every year, millions of Americans visit their healthcare provider for respiratory diseases such as allergies, asthma, bronchitis, common cold, chronic obstructive pulmonary disease (COPD), and pneumonia.
Currently, more than 25 million people in the United States have asthma. Approximately 14.8 million adults have been diagnosed with COPD, and approximately 12 million people have not yet been diagnosed. The burden of respiratory diseases affects individuals and their families, schools, workplaces, neighborhoods, cities, and states. Because of the cost to the health care system, the burden of respiratory diseases also falls on society; it is paid for with tax dollars, higher health insurance rates, and lost productivity. Annual healthcare expenditures for asthma alone are estimated at $20.7 billion.
The purpose of the respiratory system is to perform gas exchange. Pulmonary ventilation provides air to the alveoli for this gas exchange process. At the respiratory membrane, where the alveolar and capillary walls meet, gases move across the membranes, with oxygen entering the bloodstream and carbon dioxide exiting. Through this mechanism, blood is oxygenated, and carbon dioxide, the waste product of cellular respiration, is removed from the body. Portions of the respiratory system are also used for non-vital functions, such as sensing odors and speech production, and for straining, such as during childbirth or coughing.
Understanding these basics will help us appreciate the importance of managing and treating respiratory conditions effectively. Next, we can explore the various medications used to treat these conditions, including their mechanisms of action, uses, and side effects.
Figure 1 Major Respiratory Structures: The major respiratory structures span the nasal cavity to the diaphragm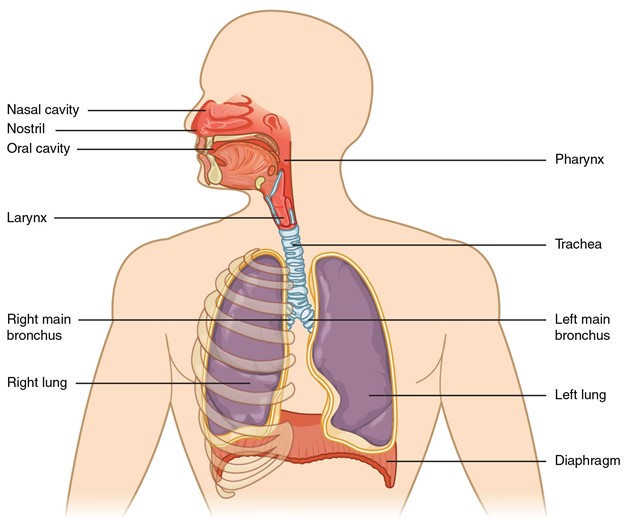
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone includes the organs and structures not directly involved in gas exchange, while gas exchange occurs in the respiratory zone.
Conducting Zone
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air. Several structures within the conducting zone perform other functions as well. For example, the epithelium of the nasal passages is essential to sensing odors, and the bronchial epithelium that lines the lungs can metabolize some airborne carcinogens.
The cilia of the respiratory epithelium help remove the mucus and debris from the nasal cavity with a constant beating motion, thus sweeping materials toward the throat to be swallowed. Interestingly, cold air slows the movement of the cilia, resulting in the accumulation of mucus that may, in turn, lead to a runny nose during cold weather. This moist epithelium functions to warm and humidify incoming air—capillaries located just beneath the nasal epithelium warm the air by convection.
Bronchial Tree
The trachea branches into the right and left primary bronchi at the carina. A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi. The main function of the bronchi, like other conducting zone structures, is to provide a passageway for air to move into and out of each lung. In addition, the mucous membrane traps debris and pathogens.
A bronchiole branches from the tertiary bronchi. Bronchioles, which are about 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which lead to the structures of gas exchange. There are more than 1,000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage like those of the bronchi. This muscular wall can change the size of the tubing to increase or decrease airflow through the tube.
Respiratory Zone
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole, which then leads to an alveolar duct, opening into a cluster of alveoli.
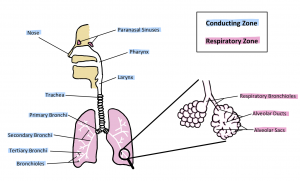
The Respiratory Zone. Bronchioles lead to alveolar sacs in the respiratory zone where gas exchange occurs.
Alveoli
An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange.
Respiratory Rate and Control of Ventilation
Breathing usually occurs without thought, although at times, you can consciously control it, such as when you swim underwater, sing a song, or blow bubbles. The respiratory rate is the total number of breaths, or respiratory cycles, that occur each minute. Respiratory rate can be an important indicator of disease, as the rate may increase or decrease during an illness. The respiratory rate is controlled by the respiratory center located within the medulla oblongata in the brain, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood.
The normal respiratory rate of a child decreases from birth to adolescence. A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute, but by the time a child is about 10 years old, the normal rate is closer to 18 to 30. By adolescence, the normal respiratory rate is similar to that of adults, 12 to 18 breaths per minute.
Neurons that stimulate the muscles of the respiratory system are responsible for controlling and regulating pulmonary ventilation. The major brain centers involved in pulmonary ventilation are the medulla oblongata and the pontine respiratory group.
II. Disease of the respiratory system
The respiratory system can be affected by a variety of diseases, ranging from acute infections to chronic conditions and structural abnormalities. These diseases can impact any part of the respiratory tract, from the upper airways to the alveoli in the lungs. Here’s an overview of some common and significant respiratory diseases:
Asthma
Asthma is a common condition that affects the lungs in both adults and children. Approximately 8.2 percent of adults (18.7 million) and 9.4 percent of children (7 million) in the United States suffer from asthma. In addition, asthma is the most frequent cause of hospitalization in children.
Asthma is a chronic disease characterized by inflammation, edema, and bronchospasm of the airways, which inhibits air from entering the lungs. In addition, excessive mucus secretion can occur, which further contributes to airway blockage. Cells of the immune system, such as eosinophils and mononuclear cells, may also be involved in infiltrating the walls of the bronchi and bronchioles.
Bronchospasms occur periodically and lead to an “asthma attack.” An attack may be triggered by environmental factors such as dust, pollen, pet hair, dander, weather changes, mold, tobacco smoke, respiratory infections, exercise, and stress.
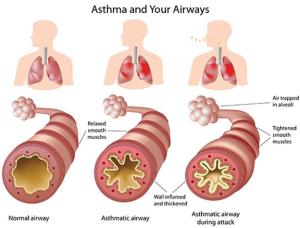
An illustration of how asthma affects the airways.
Symptoms of an asthma attack involve coughing, shortness of breath, wheezing, and tightness of the chest. Symptoms of a severe asthma attack that require immediate medical attention include difficulty breathing that results in cyanotic lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety.
The severity of the condition, frequency of attacks, and identified triggers influence the type of medication that an individual may require. Long-term treatments are used for patients with severe asthma. Short-term, fast-acting drugs are used to treat an asthma attack and are typically administered via an inhaler or nebulizer.
Bronchitis
Bronchitis is an inflammation of the lining of the bronchial tubes, which carry air to and from the lungs. People who have bronchitis often cough up thickened mucus, which can be discolored. Bronchitis may be either acute or chronic.
Acute bronchitis, also called a chest cold, is very common. It often develops from a cold or other respiratory infection and usually improves within a week to 10 days without lasting effects, although the cough may linger for weeks.
Chronic bronchitis, a more serious condition, is a constant irritation or inflammation of the lining of the bronchial tubes, often caused by smoking. It is one of the conditions included in COPD.
Symptoms for either acute bronchitis or chronic bronchitis may include:
- Cough
- Production of mucus (sputum), which can be clear, white, yellowish-gray, or green in color — rarely, it may be streaked with blood.
- Fatigue
- Shortness of breath
- Slight fever and chills
- Chest discomfort
III. Medication for the Management of Respiratory Disease.
The management of respiratory diseases often involves a combination of medications that target different aspects of the condition, such as reducing inflammation, relaxing airway muscles, treating infections, or addressing symptoms like cough and mucus production. Here’s an overview of common medications used for respiratory diseases mentioned above:
Beta 2 Adrenergic Agonist
Albuterol is an example of a short-acting Beta 2 Adrenergic agonist. It can also be used as a short and long-term control inhaler. As a rapid-acting short term medication, it is known as a “rescue” inhaler.
Mechanism of Action: Stimulates dilation of smooth muscle in bronchioles and bronchi.
Indications for Use: Beta 2 adrenergic agonist is used for the treatment or prevention of bronchospasms for individuals with asthma, bronchitis, emphysema, exercise-induced bronchospasms and other diseases of the lungs.
Adverse/Side Effects: palpitations, tachycardia, excessive cardiac and central nervous system stimulation, anxiety/nervousness, excitability, tremors.
Types of Beta 2 Adrenergic Medications: There are two types of Beta 2 adrenergic agonist medications: 1). Short-Acting Beta 2 Agonist (SABAs)-these help to provide rapid relief of sudden and severe symptoms such as wheezing and shortness of breath. Albuterol falls in this category. 2). Long-Acting Beta 2 Agonist (LABAs)-these medications are used for maintenance and long-term management of the conditions listed above, and can provide bronchodilation for longer periods of time. These medications are often mixed with inhaled corticosteroids. An example of this type would be salmeterol.
Beta 2 Adrenergic Medications across the Life Span: beta 2 adrenergic agonists can be used for children, adults and older adults to prevent exacerbations, manage acute symptoms, improve lung function, and to improve the quality of life for individuals who are living asthma and other respiratory conditions. Precaution must be used for each population when prescribing and administering this classification of medications.
Patient Teaching & Education: The patient should be instructed to avoid excessive caffeine intake, to avoid triggers that can lead to an acute respiratory episode (e.g., outdoor allergens such as pollen, mold, smoking etc.). The medication must be taken exactly as prescribed, if there medications interferes with their ability to perform activities of daily living, they should notify their healthcare provider. The patient should keep a log history of frequency of use and intensity of their condition and report side/adverse effects such as allergic reactions or effects that are continuous or prolong, such as palpitations, nervousness/anxiety. Patient should be properly trained on how to use a metered dose inhaler and if a spacer device is needed, they should know how to use it as well.
Anticholinergics
Ipratropium is an example of a short-acting anticholinergic. Tiotropium is an example of a long-acting anticholinergic. Additional information regarding anticholinergics can be found in the “Autonomic Nervous System” chapter.
Mechanism of Action: Anticholinergics block the action of acetylcholine in bronchial smooth muscle, which reduces Broncho-constrictive substance release.
Indications for Use: Anticholinergics are used for maintenance therapy of bronchoconstriction associated with asthma, chronic bronchitis, and emphysema.
Adverse/Side Effects: Anticholinergics should be used with caution with the elderly, as they can cause cough, drying of the nasal mucosa, nervousness, nausea, GI upset, headaches, and dizziness.
Anticholinergic Drugs across the Life Span: Wheezing is an indication of the use of anticholinergic drugs, but although we do see wheezing in infancy, using these drugs remains controversial. Most wheezing in infancy is in response to viral infections.
Patient Teaching & Education: The patient should be instructed to use the inhaler as directed and be careful not to exceed dosage recommendations. They should receive education regarding the onset of medication and differences in usage for short- and long-acting anticholinergics. Patients with certain diseases should not use anticholinergics including Myasthenia gravis, hyperthyroidism, glaucoma, enlarged prostate, hypertension, urinary tract blockage, tachycardia and heart failure. Some long-acting anticholinergics may cause signs of angioedema, and the healthcare provider should be notified if this occurs.
Xanthine Derivatives
Exemplar: Theophylline.
Mechanism of Action: Theophylline relaxes bronchial smooth muscle by inhibition of the enzyme phosphodiesterase and suppresses airway responsiveness to stimuli that cause bronchoconstriction.
Indications for Use: Theophylline is used for the long-term management of persistent asthma that is unresponsive to beta-agonists or inhaled corticosteroids.
Adverse/Side Effects: Theophylline can cause nausea, vomiting, CNS stimulation, nervousness, and insomnia.
Nursing Considerations Across a Life Span: The long-term use of these drugs with childhood asthma needs to be reassessed. Although they are considered a first-line preventer for alleviating symptoms in children, evidence questions their reliability. Currently, used as prescribed by a medical professional, they are deemed safe; however, as research advances, these indications may change. Further research is indicated.
Patient Teaching & Education: Patients should be sure to take medications as prescribed and at appropriate intervals. They should avoid irritants and drink fluids to help thin secretions. Patients will need to have their serum blood levels tested every six to twelve months.
Corticosteroids
Corticosteroids can be prescribed in a variety of routes. Fluticasone is an example of a commonly used inhaled corticosteroid; prednisone is an example of a commonly used oral corticosteroid; and methylprednisolone is a commonly used IV corticosteroid. Additional information about corticosteroids and potential adrenal effects is located in the “Endocrine” chapter.
Mechanism of Action: Fluticasone is a locally-acting anti-inflammatory and immune modifier. The nasal spray is used for allergies, and the oral inhaler is used for long-term control of asthma. Fluticasone is also used in a combination product with salmeterol. It decreases the frequency and severity of asthma attacks and improves overall asthma symptoms. Oral prednisone prevents the release of substances in the body that cause inflammation. It also suppresses the immune system. Methylprednisolone IV prevents the release of substances in the body that cause inflammation. It also suppresses the immune system. Methylprednisolone requires reconstitution before administration.
Indications for Use: Fluticasone inhalers are used to prevent asthma attacks. In respiratory conditions, oral prednisone is used to control severe or incapacitating allergic conditions that are unresponsive to adequate trials of conventional treatment for seasonal or perennial allergic rhinitis, bronchial asthma, contact dermatitis, atopic dermatitis, serum sickness, and drug hypersensitivity reactions. Methylprednisolone IV is used to rapidly control these same conditions.
Nursing Considerations Across the Lifespan: Fluticasone is safe for children aged 4 years and older. Prednisone and methylprednisolone are safe for all ages. Watch for potential mood changes such as irritability and possible hyperactivity in children. Short term use can also lead to increase in blood pressure and blood sugar levels.
Adverse/Side Effects: Fluticasone can cause hoarseness, dry mouth, cough, sore throat, and oropharyngeal candidiasis. Patients should rinse their mouths after use to prevent candidiasis (thrush). Prednisone and methylprednisolone: See more information about the adverse effects of corticosteroids in the Endocrine chapter. Cardiovascular symptoms can include fluid retention, edema, and hypertension. Imbalances such as hypernatremia (↑Na), hypokalemia (↓ K+), and increased blood glucose with associated weight gain can occur. CNS symptoms include mood swings and euphoria. GI symptoms can include nausea, vomiting, and GI bleeding. In long-term therapy, bone resorption occurs, which increases the risk for fractures; the skin may bruise easily and become paper thin; wound healing is delayed; infections can be masked; and the risk for infection increases. Long-term corticosteroid therapy should never be stopped abruptly because adrenal insufficiency may occur.
Patient Teaching & Education: Patients should be advised that corticosteroids are not used to treat an acute asthma attack. They can cause immunosuppression and suppress signs of infection. Corticosteroids can also cause an increase in blood glucose levels. Patients may experience weight gain, swelling, increased fatigue, bruising, and behavioral changes. These occurrences should be reported to one’s healthcare provider.
Knowledge Check: Respiratory Medication Quiz
Clinical Application: Provide Instructions ( Ask the same questions as the classroom project exercise)
Media Attributions
- Picture1
- Conducting-and-Respiratory-Zones-300×181
- Picture2

