4 Defense and Immunity: Infection and Antimicrobials-Bacteria and Antibacterials
Understanding the fundamental concepts of defense and immunity, the pathophysiology of infection, and pharmacologic principles is essential for nurses to provide comprehensive patient care. The immune system, comprising innate and adaptive immunity, protects against pathogens through immediate, non-specific, targeted, long-term responses. Infections arise when pathogens invade, evade the immune system, and replicate, leading to tissue damage. Recognizing early signs of infection and understanding its progression are crucial for timely interventions. Pharmacologic management, involving antibiotics, antivirals, antifungals, and antiparasitics, requires knowledge of pharmacokinetics and pharmacodynamics for safe and effective administration.
Additionally, awareness of antimicrobial resistance and stewardship principles is vital. Integrating these concepts into nursing practice allows for accurate assessments, effective interventions, patient education, and collaboration with healthcare teams, ultimately enhancing patient care quality and outcomes. This chapter presents several units: a) normal mechanisms of defense and immunity, b) concepts of infection, c) considerations for antimicrobial therapy, and d) pharmacologic concepts of antimicrobial therapy. Clinical decision-making learning activities are integrated throughout this chapter.
The concepts of defense and immunity involving antimicrobials will be divided in two parts. This chapter focuses on the the foundational concepts of pathophysiology of infections to and foundations of pharmacology related to antimicrobial therapy. The following chapter goes into more details of pharmacologic therapy.
Learning Objectives
- Identify populations who have an increased risk of infection.
- Describe common pathogens and methods of infection control.
- Distinguish between antimicrobial agents in terms of mechanism of action, indication for use, adverse effects, and implications for the nursing process.
- Apply knowledge of ways to minimize the emergence of drug-resistant microorganisms.
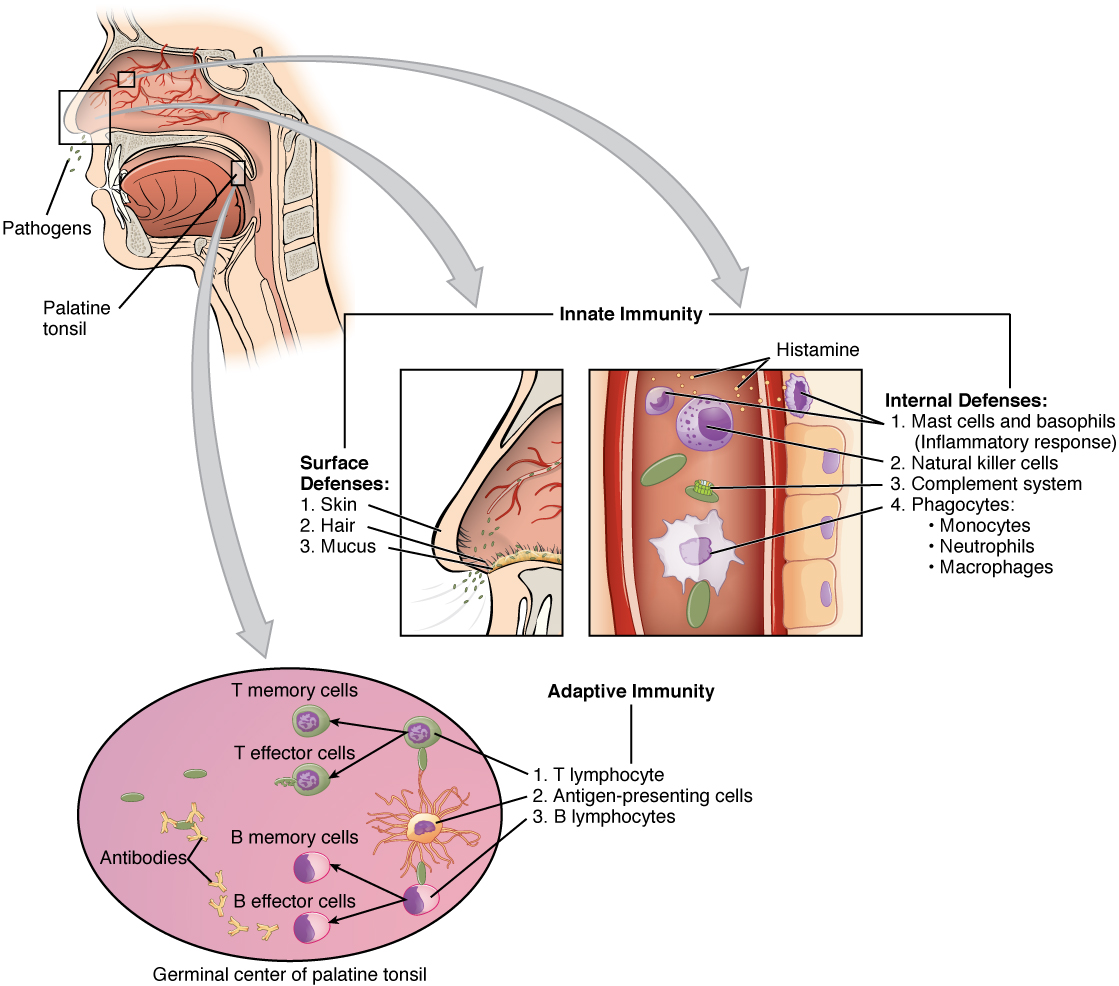
The human immune system comprises a complex network of cells, tissues, and organs that work collaboratively to defend the body against pathogens such as bacteria, viruses, fungi, and parasites. The immune system’s defense mechanisms are categorized into two main types: innate (nonspecific) immunity and adaptive (specific) immunity.
A. Innate Immunity is the first line of defense and provides a rapid but nonspecific response to pathogens. It includes physical barriers, chemical barriers, and cellular defenses.
1. Physical Barriers: The skin and mucous membranes act as physical barriers to prevent the entry of pathogens. The skin provides a tough, impermeable barrier, while mucous membranes trap pathogens in mucus and are equipped with cilia to expel them (Delves et al., 2017).
2. Chemical Barriers: Secretions such as saliva, tears, and stomach acid contain antimicrobial enzymes like lysozyme, which can break down bacterial cell walls. The stomach’s acidic environment also destroys many ingested pathogens (Murphy & Weaver, 2016).
3. Cellular Defenses: Various cells play crucial roles in innate immunity, including:
- Phagocytes: Neutrophils and macrophages ingest and destroy pathogens through phagocytosis. These cells recognize pathogens through pattern recognition receptors (PRRs) that detect pathogen-associated molecular patterns (PAMPs) (Janeway et al., 2001).
- Natural Killer (NK) Cells: NK cells can identify and kill virus-infected cells and tumor cells by inducing apoptosis. Apoptosis is a form of programmed cell death that occurs in multicellular organisms. It’s a highly regulated and controlled process that leads to the elimination of cells without releasing harmful substances into the surrounding area. Apoptosis plays a crucial role in maintaining the health of an organism by removing damaged, diseased, or unnecessary cells. It involves a series of biochemical events leading to characteristic cell changes (such as cell shrinkage, nuclear fragmentation, chromatin condensation, and chromosomal DNA fragmentation) and ultimately, death ( Elmore, 2007).
- Dendritic Cells: These cells act as messengers between innate and adaptive immunity by capturing antigens and presenting them to T cells (Steinman & Hemmi, 2006).
B. Adaptive Immunity is characterized by its specificity and memory. It involves lymphocytes, including B cells and T cells, and is activated when the innate immune response is insufficient.
- B Cells and Antibodies: B cells are responsible for humoral immunity. Upon encountering an antigen, B cells differentiate into plasma cells that produce antibodies specific to that antigen. Antibodies neutralize pathogens, optimize them for phagocytosis, and activate the complement system, leading to pathogen lysis (Murphy & Weaver, 2016).
- T Cells: T cells are involved in cell-mediated immunity. There are two main types:
-
- Helper T Cells (Th cells): These cells assist other immune cells by releasing cytokines that enhance the immune response. The cells are critical for activating B cells and cytotoxic T cells (Murphy & Weaver, 2016).
- Cytotoxic T Cells (Tc cells): Tc cells directly kill infected or cancerous cells by inducing apoptosis. They recognize antigens presented by major histocompatibility complex (MHC) class I molecules on the surface of infected cells (Janeway et al., 2001).
3. Memory Cells: After an initial infection, both B and T cells can form memory cells. These memory cells provide a faster and more robust response upon subsequent exposures to the same pathogen, which is the basis for long-lasting immunity and the effectiveness of vaccines (Plotkin, 2010).
II. Pathophysiology of Infection and Related Concepts
Infection is the invasion and multiplication of microorganisms such as bacteria, viruses, fungi, or parasites in the body, which may lead to tissue damage and an immune response. Infections can be localized to a particular part of the body or systemic, spreading throughout the body. The outcome of an infection can vary from mild to severe, and in some cases, it can be life-threatening. The body typically responds to infections with an immune response to fight off the invading pathogens (Giddens, 2017). This unit provides a basic introduction to the concept of infection related to pharmacology. The example concept map below summarizes the key information necessary to understand infection. You can revisit this map after you have completed the chapter. The information for the map was informed by several resources (Giddens, 2017). This unit provides a basic introduction to the concept of infection related to pharmacology. The example concept map below summarizes the key information necessary to understand infection. 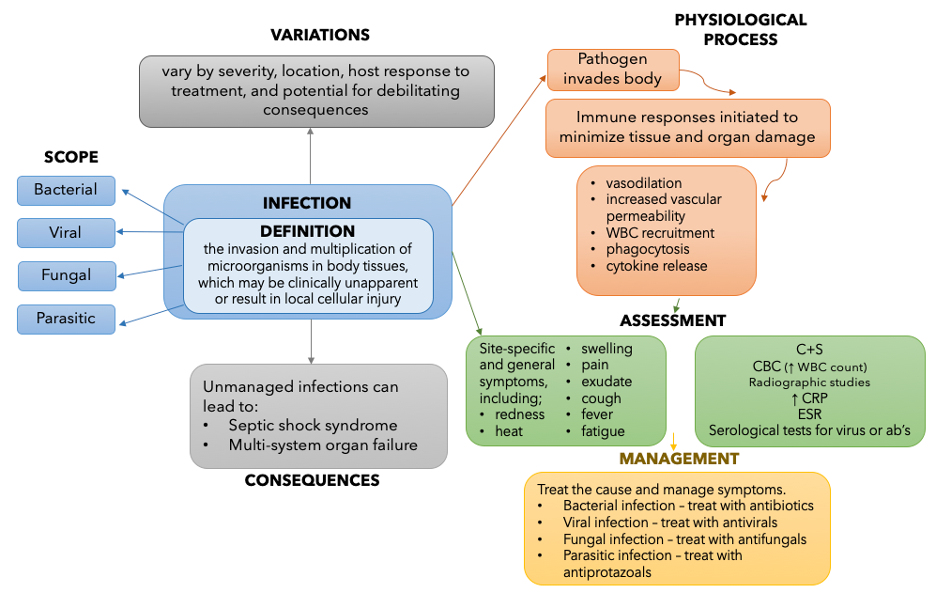
Nurses need to understand the basics of microbiology before learning the pharmacologic concepts of antimicrobial therapy. Microorganisms include bacteria, viruses, fungi, and parasites. Bacteria are found in nearly every habitat on earth, including within and on humans. Most bacteria are harmless or considered helpful, but some are pathogens. A pathogen is defined as an organism causing disease to its host. Pathogens, when overgrown, can cause significant health problems or even death for your patients.
The pathophysiology of infection involves a complex interplay between the invading pathogen and the host’s immune system. This process encompasses several stages: pathogen entry, immune response activation, pathogen dissemination, and resolution or progression to chronic infection.
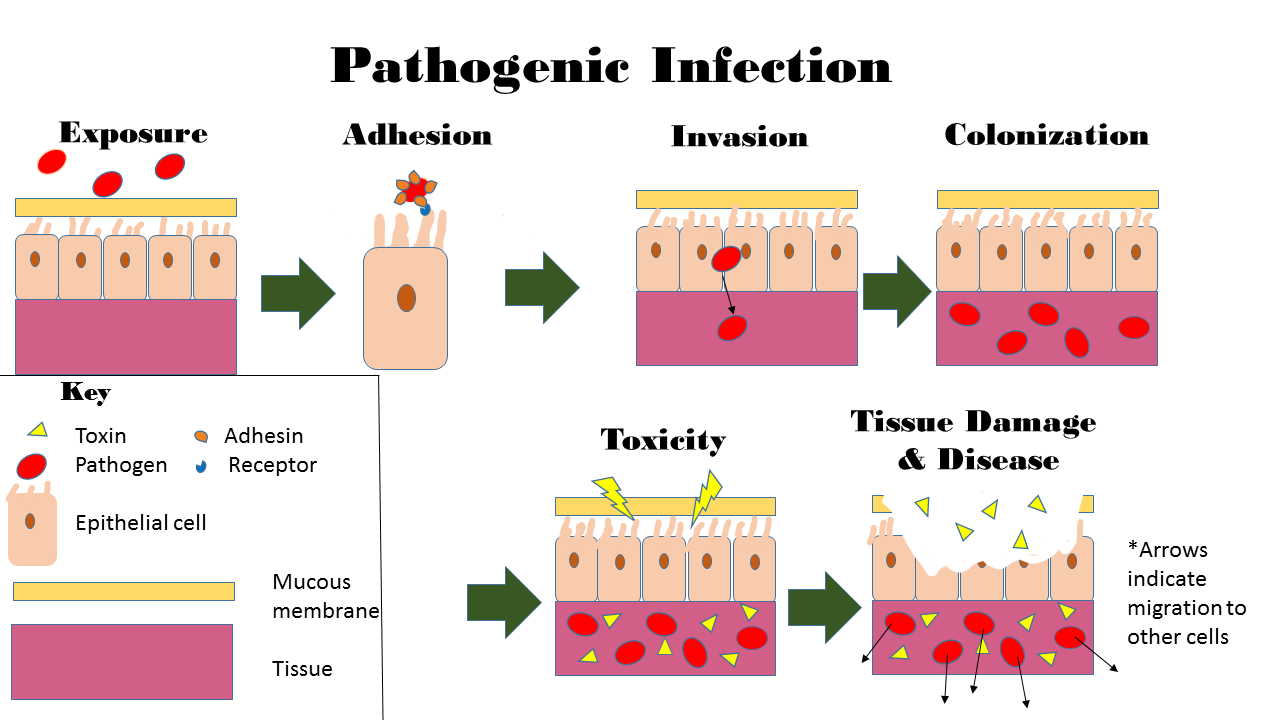
Pathogen Entry and Colonization
The initial step in infection is the pathogen’s entry into the host. Pathogens can enter the body through various portals, including the respiratory tract, gastrointestinal tract, urogenital tract, and breaks in the skin (Murray, Rosenthal, & Pfaller, 2016). For instance, respiratory pathogens like influenza viruses enter through inhalation, while gastrointestinal pathogens like Salmonella species enter via ingestion of contaminated food or water. Once inside the host, pathogens must adhere to host cells to establish an infection. Specific interactions mediate this adhesion between pathogen surface molecules (adhesins) and host cell receptors. For example, the influenza virus uses its hemagglutinin protein to bind to sialic acid residues on the surface of respiratory epithelial cells ( Murphy & Weaver, 2016).
Immune Response Activation
Following entry and colonization, the host immune system detects the presence of the pathogen. Innate immunity is the first line of defense, involving physical barriers, chemical mediators, and cellular responses. Pathogen-associated molecular patterns (PAMPs) on the surface of pathogens are recognized by pattern recognition receptors (PRRs) on host cells, such as Toll-like receptors (TLRs) and NOD-like receptors (NLRs) (Abbas, Lichtman, & Pillai, 2018). Activation of PRRs leads to the production of pro-inflammatory cytokines, chemokines, and other mediators that recruit immune cells to the site of infection. Neutrophils and macrophages are among the first responders, phagocytosing pathogens and releasing antimicrobial substances. Additionally, the complement system is activated, resulting in opsonization, inflammation, and direct lysis of pathogens (Murphy & Weaver, 2016).
Pathogen Dissemination
If the innate immune response is insufficient to contain the infection, pathogens may disseminate to other tissues and organs. This dissemination can occur via the bloodstream (hematogenous spread) or lymphatic system. For example, the bacterium Neisseria meningitidis can cross the blood-brain barrier and cause meningitis (Murray, Rosenthal, & Pfaller, 2016). Pathogens have evolved mechanisms to evade the host immune system and facilitate dissemination. These mechanisms include antigenic variation, inhibition of phagosome-lysosome fusion, and production of immune-modulatory molecules. For instance, Mycobacterium tuberculosis, the causative agent of tuberculosis, can survive within macrophages by preventing phagosome-lysosome fusion (Janeway et al., 2001).
Host Response and Tissue Damage
The adaptive immune response is crucial for controlling and eliminating infections, bypassing innate immune defenses. T and B lymphocytes recognize specific antigens presented by antigen-presenting cells (APCs). Helper T cells (Th cells) orchestrate the immune response by secreting cytokines that activate other immune cells. In contrast, cytotoxic T cells (Tc cells) directly kill infected cells (Abbas, Lichtman, & Pillai, 2018). B cells differentiate into plasma cells that produce antibodies. These antibodies neutralize pathogens, promote opsonization, and activate the complement system. However, the immune response can also contribute to tissue damage. For example, excessive inflammation and cytokine release can lead to a “cytokine storm,” causing widespread tissue injury and organ failure, as seen in severe cases of COVID-19 (Murphy & Weaver, 2016).
Resolution or Chronic Infection
The outcome of an infection depends on the balance between pathogen virulence and host immune defenses. Successful resolution occurs when the immune system eliminates the pathogen and repairs damaged tissues. Memory T and B cells are generated, providing long-lasting immunity against future infections by the same pathogen (Murphy & Weaver, 2016). Infections can sometimes become chronic, with pathogens persisting in the host despite the immune response. Chronic infections can result from various factors, including immune evasion by the pathogen, host immunodeficiency, or biofilm formation. Chronic infections can lead to ongoing inflammation, tissue damage, and complications such as cancer (Murray, Rosenthal, & Pfaller, 2016).
Clinical Exercise: The case of a community acquired bacterial infection in an older adult
Name: M.S.; Age: 78 years old; Gender: Female; Background: M.S. is a retired school teacher who lives alone. She has a history of hypertension and type 2 diabetes, both of which are managed with medication. She has recently experienced a decline in her mobility due to osteoarthritis, leading to less frequent outings and physical activity. She has not received her annual flu vaccine this year and missed the pneumococcal vaccine.
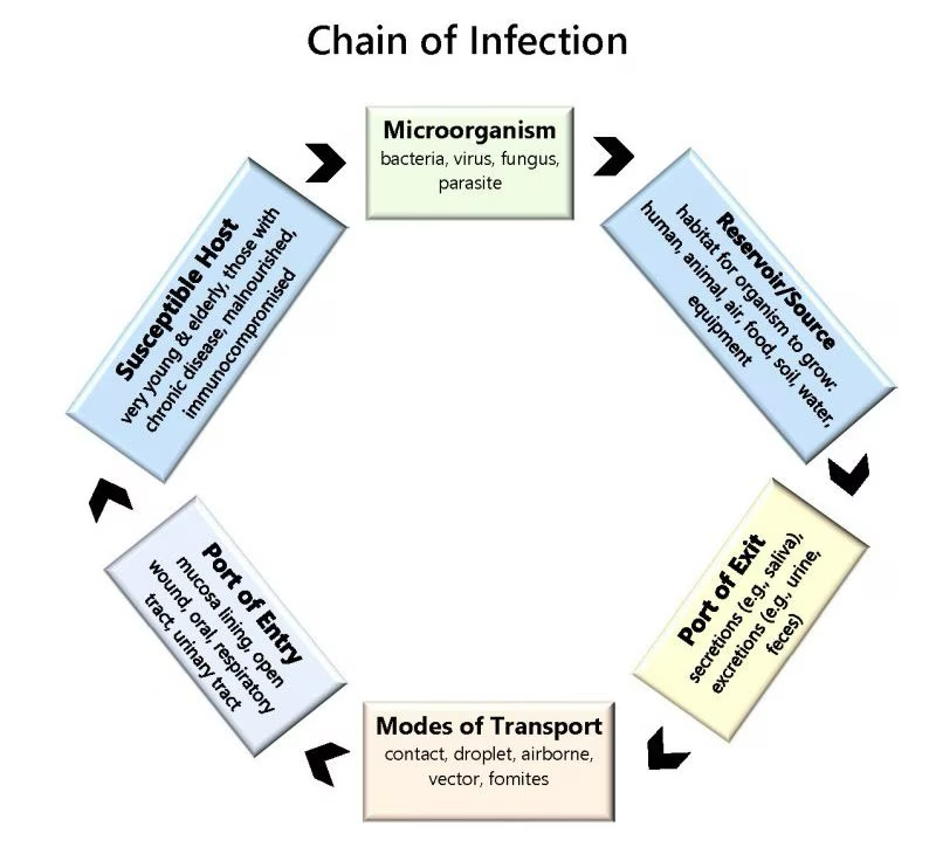
The chain of infection describes how infections spread from one host to another. Understanding this chain will guide healthcare workers in implementing effective infection control measures.
- Infectious Agents are pathogens (bacteria, viruses, fungi, parasites) that cause diseases, such as Influenza, E. coli, Mycobacterium tuberculosis, and other organisms mentioned in the previous section. To break the link to the chain, control measures will include identifying the pathogen and using antimicrobial agents (antibiotics, antivirals) (CDC, 2022). The use of antimicrobials will be discussed in subsequent units.
- Reservoirs are habitats where pathogens, such as humans, animals, and the environment (water, soil), live, grow, and multiply.
- Control measures: Proper sanitation, health screenings, and environmental controls (clean water supply and proper waste disposal)( WHO, 2022).
- Portals of Exit are the paths by which the pathogen leaves the reservoir, such as the respiratory tract (coughing, sneezing), gastrointestinal tract (feces), and blood (needles, insect bites).
- Control measures: Covering the mouth and nose when sneezing/coughing, using personal protective equipment (PPE), and properly disposing of waste (Mayo Clinic, 2022).
- Mode of Transmission is how the pathogen is transmitted from the reservoir to a susceptible host. The modes of transmission are:
- Direct contact: Person-to-person (touching, kissing)
- Indirect Contact: Through an intermediate object (fomite)
- Droplet: Respiratory droplets (coughing, sneezing)
- Airborne: Aerosols that remain in the air
- Vector-borne: Via animals or insects (mosquitoes, ticks)
- Control measures include hand hygiene, Disinfecting surfaces, Using barriers (masks, gloves), and pest control (APIC, 2021).
- Portal of Entry: The path by which the pathogen enters the new host.
- Examples: Respiratory tract, gastrointestinal tract, broken skin, mucous membranes.
- Control measures: Maintaining skin integrity, using antiseptics, and practicing safe injections (Johns Hopkins Medicine, 2021).
- Susceptible Host Definition: An individual at risk of infection due to lack of immunity or other factors.
- Factors Influencing Susceptibility: Age (infants, elderly), health status (immunocompromised, chronic diseases), nutritional status, and genetics.
- Control Measures: vaccination, healthy lifestyle (nutrition, exercise), and managing underlying conditions(CDC, 2022).
Infection Control Measures: Breaking the Chain
Effective infection control involves several strategies to prevent the transmission of pathogens, particularly in healthcare settings:
- 1. Hand Hygiene: Regular hand washing with soap and water or using alcohol-based hand sanitizers is the most effective way to prevent the spread of infections. Healthcare workers should follow hand hygiene protocols before and after patient contact (WHO, 2009).
- Personal Protective Equipment (PPE): Gloves, gowns, masks, and eye protection help protect healthcare workers and patients from infection. Appropriate PPE use is essential, especially during procedures that generate aerosols or involve contact with body fluids (CDC, 2022).
- Vaccination: Immunization is a critical component of infection control. Vaccines prevent the spread of infectious diseases such as influenza, measles, and COVID-19. Healthcare facilities should ensure that patients and staff are updated with recommended vaccines (WHO, 2021).
- Environmental Cleaning and Disinfection: Regular cleaning and disinfection of surfaces, especially in high-touch areas, reduce the risk of pathogen transmission. This includes the use of disinfectants effective against a broad range of pathogens (CDC, 2022).
- Isolation and Quarantine: Patients with infectious diseases should be isolated to prevent transmission to others. Quarantine measures may be necessary for individuals exposed to contagious diseases until it is clear they are not infected (CDC, 2022).
- Antimicrobial Stewardship: Responsible use of antibiotics and other antimicrobial agents is vital to prevent the development of resistance. This includes prescribing antibiotics only when necessary and completing the prescribed course (WHO, 2021).
Understanding common pathogens and implementing robust infection control measures are crucial for preventing the spread of infectious diseases. Continued education, adherence to guidelines, and advancements in medical research are essential to protect public health.
Preventing Transmission of Infectious Conditions: Watch the video below and answer the following questions:
III. Conditions and Diseases Related to Infection
Humans are constantly exposed to many microorganisms, such as bacteria, viruses, parasites, and fungi. Although many microorganisms do not pose a health threat to humans, some cause human disease and are known as pathogens. An individual’s immune system can typically rid the body of pathogens without developing an infection. An infection occurs when a susceptible host is invaded by a pathogen that multiplies and causes disease.
- Bacterial Infections
This section presents common bacterial infections that nurses will see in the hospital and the community. Bacteria are one-celled organisms without a true nucleus or cellular organelles. They synthesize deoxyribonucleic acid (DNA), ribonucleic acid (RNA), and proteins and can reproduce independently, but they require a host for a suitable environment for multiplication. Bacteria cause cellular injury by releasing toxins that are either exotoxins (enzymes released by gram-positive bacteria into the host) or endotoxins (part of the bacterial cell wall of gram-negative bacteria that can cause damage to the host even if the bacteria are dead). Diseases caused by bacterial invasion depend on the type of bacterial pathogen and the area of the body that is primarily invaded.
Review your knowledge of bacteria by using this resource: Overview of Bacteria.
Common bacterial infections
- Salmonella is a type of infection often described as food poisoning. It causes severe stomach cramps, fever, diarrhea, and vomiting. Salmonella is caused by a non-typhoidal salmonellae bacteria found in the intestinal tracts of humans and other animals. The most recognized method of infection is through undercooked poultry. Salmonella strains sometimes cause infection in urine, blood, bones, joints, or the nervous system (spinal fluid and brain) and can cause severe disease.
- Escherichia coli (E. coli) causes gastrointestinal (GI) distress. The infection usually resolves on its own, but if it affects the kidney, it can be severe or even fatal. E. Coli bacteria commonly spread through contaminated food (typically meat products, but sometimes even via uncooked vegetables).
- Tuberculosis (TB) is a highly contagious disease caused by the Mycobacterium tuberculosis bacteria. It most commonly causes a lung infection and rarely affects the brain. Common symptoms of TB include cough, chest pain, weakness, weight loss, fever, and lack of appetite. Although the incidence of active TB disease in the overall Canadian population has been decreasing over time and is among the lowest in the world, high rates persist among Aboriginal peoples and foreign-born individuals.
- Methicillin-resistant Staphylococcus aureus (MRSA) is an antibiotic-resistant bacteria that can be deadly, particularly in people with compromised immune systems. Staphylococcus bacteria usually live on the skin and in the nose, usually without causing problems. But if these bacteria become resistant to antibiotics, they can cause serious infections, especially in people who are ill or weak. Symptoms of MRSA depend on where the infection is – for example, if MRSA is causing an infection in a wound, that skin area may have purulent drainage and may be red, tender, and warm to the touch. MRSA differs from other types of staphylococcus because it cannot be treated with specific antibiotics, such as methicillin, making treatment complex and prolonging hospitalization. MRSA can be spread by contact with contaminated persons or through contaminated objects. It is a common hospital-acquired infection.
- Clostridium difficile (C. diff) is a bacteria usually found in the intestine. For most healthy people, C. diff is not a health risk. It can cause GI illness when it overgrows due to antibiotic use or an impaired immune system. C. diff is the most frequent cause of infectious diarrhea in hospitals and healthcare facilities. Symptoms include watery diarrhea, fever, loss of appetite, nausea, and abdominal pain/tenderness. It can spread from person to person through the fecal-oral route; for example, if a health care provider does not clean their hands with soap and water after caring for a patient with C. diff, they can potentially pass on the infection to other people, they touch. It is important to note that c. diff bacterial spores cannot be killed with alcohol hand sanitizer, therefore infected persons and their care providers must always wash using soap and water, and practice frequent hand hygiene.
- Bacterial pneumonia is a lung infection that can be caused by various bacteria, including Streptococcus pneumonia (the main culprit), Haemophilus influenzae, Staphylococcus aureus, and others. Viruses and/or fungi cause some pneumonia, but bacterial pneumonia is the most common. These infections are typically spread through air particles from coughing or sneezing (droplets) and aspiration, which then leads to an infection in the respiratory tract. Pneumonia can be further divided into community-acquired, hospital-acquired (HAP) and ventilator-associated (VAP). Community-acquired bacterial pneumonia is less likely to involve multi-drug resistant bacteria and is usually less severe than HAP and VAP.
- Heliobacter pylori (H. pylori) is a bacteria associated with stomach ulcers and chronic gastritis. The environment of the GI system can change due to reflux, acidity, and smoking, which predisposes individuals to this bacterial infection. H. pylori exists in the stomachs of approximately 50% of the population, typically causing no harm. Issues arise when H. pylori can adhere to the stomach cells and disrupt cell function, causing inflammation and ulcer formation. Symptoms of H. pylori infection include abdominal pain, loss of appetite, nausea, and bloating. In some cases, H. pylori infection can also lead to duodenal ulcers.
General symptoms of bacterial infections
Individuals of any age can develop a bacterial infection. Bacteria can infect any area of the body, including the skin, bladder, lungs, intestines, brain, and more. A bacterial infection can also spread throughout the blood, causing a condition described as sepsis. Some generalized symptoms of infection include fever, chills, and fatigue. Localized symptoms of infection can include swelling, pain at the site, redness, and organ dysfunction.
| Table 1: Systemic and Localized Symptoms of Bacterial Infection | |
| Systemic | Localized |
|
|
Knowledge Check: MS initial assessment in the ED:
•Vital Signs: Blood pressure 145/90 mmHg, pulse 102 bpm, respiratory rate 24 breaths per minute, temperature 38.6°C (101.5°F), oxygen saturation 89% on room air.
•Physical Exam: Mildly confused, uses accessory muscles to breathe, crackles heard in the lower lobes of both lungs on auscultation.
•Initial Interventions: Oxygen therapy initiated via nasal cannula at 2 L/min, increasing her saturation to 94%.
Culture and Sensitivity
When a patient presents with signs or symptoms of an infection, the work needed to identify the source of the infection begins. A culture is a test performed to examine different body substances for the presence of bacteria or fungi. These culture samples are commonly collected from a patient’s blood, urine, sputum, wound bed, etc. Nurses are commonly responsible for collecting culture samples and must be conscientious about collecting the sample before administering antibiotics. Antibiotic administration before obtaining a culture can delay the organism’s identification and complicate the patient’s recovery. Once culture samples are collected, they are incubated in a solution promoting bacterial or fungal growth and spread onto a special culture plate. Clinical microbiologists subsequently monitor the culture for signs of organism growth to aid in diagnosing the infectious pathogen. A sensitivity analysis is often performed to select an effective antibiotic to treat the microorganism. If the organism resists the antibiotics used in the test, those antibiotics will not effectively treat the patient’s infection. Sometimes, a patient may begin antibiotic treatment for an infection but will be switched to a different, more effective antibiotic based on the culture and sensitivity results.
Gram stain
A gram stain is another type of test that is used to assist in the classification of pathogens. Gram stains are useful for quickly identifying if bacteria are “gram-positive” or “gram-negative” based on the staining patterns of their cellular walls. Utilizing gram stain allows microbiologists to look for characteristic violet (Gram +) or red/pink (Gram -) staining patterns when they examine the organisms under a microscope. Identifying bacteria as gram-positive or gram-negative assists the healthcare provider in quickly selecting an appropriate antibiotic to treat the infection.
Sample Gram-Positive Infections: Figures a and b show Gram Stain Specimens of Streptococcus. Streptococcus, from the Greek word for twisted chain, is responsible for many infectious diseases in humans. It is an example of a Gram + Infection and is identified by its ability to lyse or break down red blood cells when grown on blood agar.
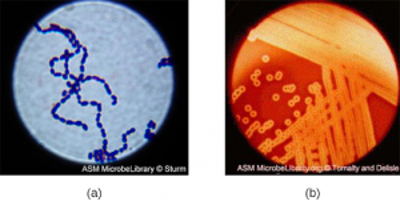
This species is considered a pyogenic pathogen because of the associated pus production observed with infections it causes (see Figure (b) for an image of Streptococcus undergoing gram staining). S. pyogenes is the most common cause of bacterial pharyngitis (strep throat); it is also a common cause of various skin infections that can be relatively mild (e.g., impetigo) or life-threatening (e.g., necrotizing fasciitis, also known as flesh-eating disease).
Staphylococcus is a second example of a Gram + bacteria. The name “Staphylococcus” comes from a Greek word for bunches of grapes, which describes their microscopic appearance in culture. Strains of S. aureus cause various infections in humans, including skin infections that produce boils, carbuncles, cellulitis, or impetigo. Many strains of S. aureus have developed resistance to antibiotics. Some antibiotic-resistant strains are designated as methicillin-resistant S. aureus (MRSA) and vancomycin-resistant S. aureus (VRSA). These strains are difficult to treat because they resist nearly all available antibiotics, not just methicillin and vancomycin. Because they are challenging to treat with antibiotics, infections can be lethal. MRSA and VRSA are also contagious, posing a severe threat in hospitals, nursing homes, dialysis facilities, and other places where there are large populations of elderly, bedridden, and/or immunocompromised individuals.
See Figure (c) for an image of Staphylococcus bacteria microscopically.
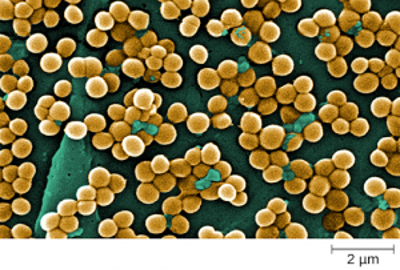
Figure c
Gram-negative bacteria often grow between aerobic and anaerobic areas (such as intestines). Some gram-negative bacteria cause severe, sometimes life-threatening disease. The genus Neisseria, for example, includes the bacteria N. gonorrhoeae, the causative agent of the sexually transmitted infection gonorrhea, and N. meningitides, the causative agent of bacterial meningitis. See Figure d for an image of Neisseria meningitides. Another common gram-negative infection seen in hospitalized patients is Escherichia coli (E. Coli). This is a frequent culprit for urinary tract infections due to its presence in the GI tract.
Figure d -Neisseria meningitides growing in colonies on a chocolate agar plate.
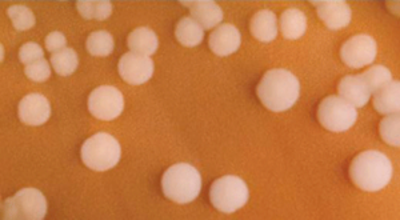
Figure (d)
Spectrum of activity is one useful factor when selecting antibiotics to treat a patient’s infection.
A narrow-spectrum antibacterial drug targets only specific subsets of bacterial pathogens. For example, some narrow-spectrum drugs target only gram-positive bacteria, but others target only gram-negative bacteria. Suppose the pathogen-causing infection has been identified in a culture and sensitivity test. In that case, it is best to use a narrow-spectrum antimicrobial and minimize collateral damage to the normal microbes.
Broad-spectrum antibacterials target various bacterial pathogens, including both gram-positive and gram-negative species. They are frequently used to cover a wide range of potential pathogens while waiting for the laboratory identification of the infecting pathogen. Broad-spectrum antimicrobials are also used for polymicrobial infections (a mixed infection with multiple bacterial species) or as prophylactic prevention of infections with surgery/invasive procedures. Finally, broad-spectrum antimicrobials may be selected to treat an infection when a narrow-spectrum drug fails because of the development of drug resistance by the target pathogen. One risk associated with broad-spectrum antimicrobials is that they will also target a broad spectrum of normal micro bacteria, potentially causing diarrhea. They also increase the risk of a superinfection, a secondary infection, in a preexisting patient. A superinfection develops when the antibacterial intended for the preexisting infection kills the protective microbiota, allowing another pathogen resistant to the antibacterial to increase and cause a secondary infection. Common examples of superinfections that develop due to antimicrobial use include yeast infections (candidiasis) and pseudomembranous colitis caused by Clostridium difficile (C-diff), which can be fatal. Probiotics, such as lactobacillus, are commonly used for individuals with C-diff to introduce normal bacteria into the gastrointestinal system and improve bowel function.
See Figure (e) for an image of C-diff microscopically.
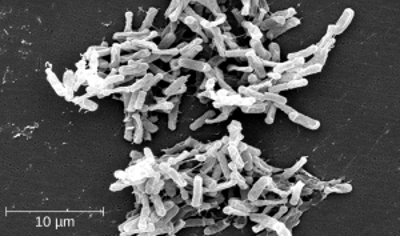
Figure (e)
Key Points:
- A broad-spectrum antibiotic will treat gram-positive and gram-negative bacteria.
- A narrow-spectrum antibiotic will treat either gram-positive or gram-negative bacteria.
If a patient is started on an antibiotic that is gram + and the culture identifies a gram – -organism, the medication will not improve the patient’s status. The selection of an incorrect antibiotic can lead to adverse reactions and increase bacterial resistance.
At times, due to the severity of the patient’s illness, a broad-spectrum antibiotic may be administered prior to receiving the culture report. Once the culture is reported, the antibiotic therapy is tailored to the patient. The nurse must review the culture results and ensure they have been communicated to the prescribing provider.
Antibacterials’ Actions – Bacteriostatic vs. Bactericidal
When a provider selects an antibacterial drug, it is important to consider how and where the drug will ultimately target the bacteria. Antibacterial drugs can be either bacteriostatic or bactericidal in their interactions with the offending bacteria. Bacteriostatic drugs cause bacteria to stop reproducing; however, they may not ultimately kill the bacteria. In contrast, bactericidal drugs kill their target bacteria.
The decision about whether to use a bacteriostatic or bactericidal drug often depends on the type of infection and the overall immune status of the patient. In a healthy patient with strong immune defenses, bacteriostatic and bactericidal drugs can effectively achieve a clinical cure. However, a bactericidal drug is essential to treat infections when a patient is immunocompromised successfully. Regardless of the patient’s immune status, life-threatening infections such as acute endocarditis require using a bactericidal drug to eliminate all offending bacteria. Watch this video: How Antibacterials Work.
Mechanism of Action
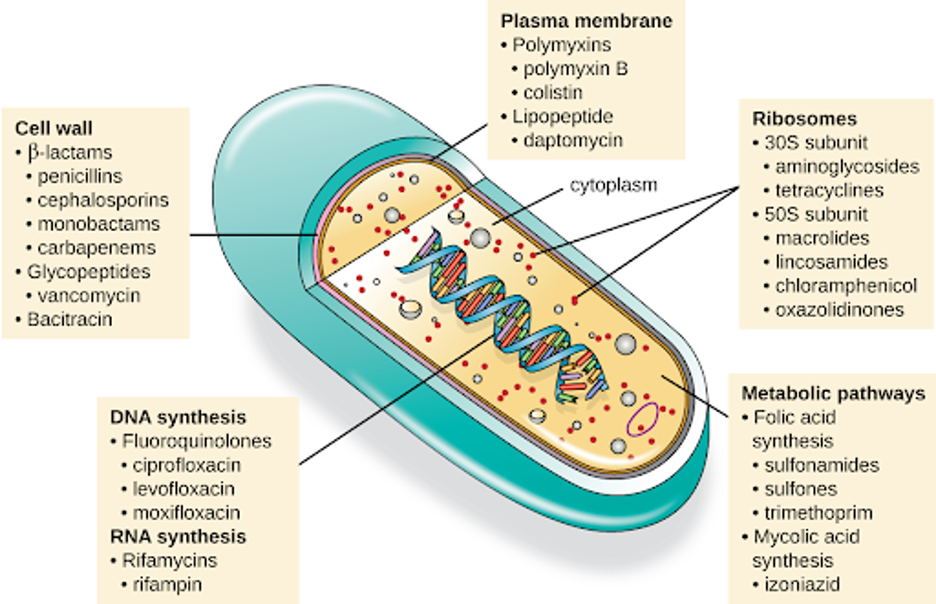
Another consideration in selecting an antibacterial drug is the drug’s mechanism of action. Mechanism of action includes:
- inhibition of cell wall synthesis (e.g. cephalosporins, penicillin, vancomycin); these antibiotics are considered to cause bactericidal effects by either producing enzymes to breakdown bacterial cell wall or to stop the production of enzymes that can make a cell wall.
- alteration in permeability of a membrane (e.g. daptomycin, nystatin); these antibiotics can cause either bacteriostatic or bactericidal effects by either increasing the permeability of the bacterial membrane or by rupturing the cell through loss of internal cellular substances.
- inhibition of protein synthesis (e.g. tetracycline, aminoglycosides); these antibiotics can be both bactericidal and bacteriostatic and are effective through their ability to interfere with protein synthesis.
- inhibition of synthesis of RNA and DNA in bacterial cell (e.g. fluoroquinolones); can bind to nucleic acid and the enzymes that are needed for production of the biomolecules.
- interference with cellular metabolism (e.g. sulfonamides); these antibiotics are bacteriostatic and interfere with the metabolic processes within cells.
Each class of antibacterial drugs has a unique mechanism of action: how a drug affects microbes at the cellular level. For example, cephalosporins act on the integrity of the cell wall. In contrast, aminoglycosides impact ribosome function and inhibit protein synthesis, which stops the proliferation of cells. See Figure f for a summary of how various antibiotics affect the cell wall, the plasma membrane, the ribosomes, the metabolic pathways, or the DNA synthesis of bacteria.
Clinical Decision-making Exercise – ANTIBIOTIC THERAPY: Complete the virtual simulations below and reflect on the following:
- Who is the patient? What is their story?
- What is the pathophysiology of the patient’s medical/surgical diagnosis?
- What are the manifestations(S/Sx) and associated functional problems of the patient?
- What medications are prescribed for the patient?
- What are the actions of the medications? How will they help the patient’s conditions/problems?
- What are the expected outcomes of the medications? What will the medication do to the body/ physiologic changes? What are the implications to the nurse’s plan of action? (Clinical Judgment, Nursing Process, safety concerns)
- What will happen to the drug when given to the patient? What are the implications to the nurse’s plan of action? (Clinical Judgment, Nursing process, safety concerns)
References:
Disease Control and Prevention. (2022). Chain of Infection. Retrieved from https://www.cdc.gov/infectioncontrol/index.html
Elmore, S. (2007). Apoptosis: A Review of Programmed Cell Death. Toxicologic Pathology, 35(4), 495-516. DOI:
Delves, P. J., Martin, S. J., Burton, D. R., & Roitt, I. M. (2017). Roitt’s Essential Immunology (13th ed.). Wiley-Blackwell.
Giddens, J. (2017). Concepts for Nursing Practice (2nd ed.). Elsevier.
Janeway, C. A., Travers, P., Walport, M., & Shlomchik, M. J. (2001). Immunobiology: The Immune System in Health and Disease (5th ed.). Garland Science.
Murray, P. R., Rosenthal, K. S., & Pfaller, M. A. (2016). Medical Microbiology (8th ed.). Elsevier
Murphy, K., & Weaver, C. (2016). Janeway’s Immunobiology (9th ed.). Garland Science.
Plotkin, S. A., Orenstein, W. A., & Offit, P. A. (2010). Vaccines (5th ed.). Saunders.
World Health Organization. (2022). Infection prevention and control. Retrieved from https://www.who.int/teams/integrated-health-services/infection-prevention-control
Attributions:
This chapter is designed as a learning material for students in fundamentals of nursing level and is largely attributed to:
https://collection.bccampus.ca/textbooks/fundamentals-of-nursing-pharmacology-a-conceptual-approach-1st-canadian-edition-bccampus-400/#license
Several topic overviews are linked to the Merck Manuals Professionals – Health & Medical InformationMerck Manualshttps://www.merckmanuals.com/
Media Attributions
- 2211_Cooperation_Between_Innate_and_Immune_Responses
- Concept Map Infection
- Pathogenic_Infection
- chain of infection
- Streptococcus
- Staphylococcus
- Neisseria
- C-diff is licensed under a CC BY (Attribution) license
- Antibiotics Mechanism of Action

