1.10. Understanding Patterns (critical thinking)
Learning Objectives
By the end of the lesson, students:
- Define key vocabulary (e.g., pattern, discrepancy, baseline, outlier) and apply these terms in a medical context.
- Identify patterns in patient symptoms through listening activities and discussion.
- Analyze patient charts to detect discrepancies or consistent trends, demonstrating an understanding of data interpretation.
- Reflect on the critical thinking process and explain how recognizing patterns and discrepancies in patient data supports effective healthcare decision-making.
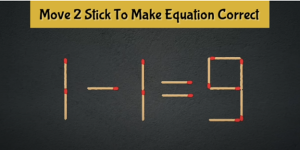
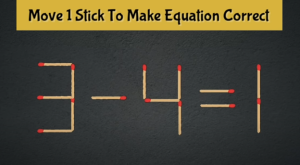
Part 1: Warm up
In pairs, solve move the stick problems.
Discussion
- What strategies did you use to figure out how to move the matchsticks and solve the problem?
- Did you approach the problem in a step-by-step way, or did you try different solutions randomly? Why?
- What challenges did you face while solving the puzzle, and how did you overcome them?
- How do you think this type of problem-solving applies to your work as a CMA?
Part 2: Critical thinking
Now, Read the below five short paragraphs and match them with the correct critical thinking skill.
Discussion
What do one need to do to develop these skills?
Part 3: Critical thinking when reviewing patient chart
Read the below patient data, and work in groups to identify discrepancies or patterns among the patient’s chief complaint, medical history, physical examination and laboratory results.
Patient Information
- Name: John Smith
- Age: 45
- Gender: Male
- Date of Birth: January 15, 1979
- Patient ID: 123456
- Date of Visit: December 10, 2024
- Primary Care Physician: Dr. Emily Johnson
Chief Complaint
- Patient presents with increased fatigue, persistent cough, and shortness of breath over the past two weeks.
Medical History
- Chronic Conditions:
- Hypertension (diagnosed 2015)
- Type 2 Diabetes Mellitus (diagnosed 2018)
- Medications:
- Lisinopril 10 mg daily
- Metformin 1000 mg twice daily
- Allergies: None reported
- Symptoms
- Duration: Symptoms have been present for approximately 2 weeks.
- Cough: Dry cough, worse at night.
- Fatigue: Notable fatigue during daily activities.
- Shortness of Breath: Occurs during exertion and while lying flat.
________________________________________
Physical Examination
- Vital Signs:
- Blood Pressure: 135/85 mmHg
- Heart Rate: 88 bpm
- Respiratory Rate: 18 breaths/min
- Temperature: 98.6°F
- Oxygen Saturation: 94% on room air
- General Appearance: Alert, but appears fatigued.
- Lungs: Mild wheezing noted upon auscultation; no crackles.
- Heart: Regular rate and rhythm; no murmurs.
- Extremities: No edema; pulses are intact.
________________________________________
Laboratory Results
- CBC (Complete Blood Count):
- Hemoglobin: 13.5 g/dL (Normal: 13.0-17.0)
- White Blood Cells: 6,500 cells/uL (Normal: 4,500-11,000)
- Platelets: 250,000 cells/uL (Normal: 150,000-450,000)
- CMP (Comprehensive Metabolic Panel):
- Glucose: 150 mg/dL (High)
- BUN: 14 mg/dL (Normal: 7-20)
- Creatinine: 0.9 mg/dL (Normal: 0.6-1.2)
- Electrolytes: Normal range
- Chest X-ray:
- Findings: Mild hyperinflation of the lungs; no acute infiltrates or effusions.
Assessment
- Primary Diagnosis: Exacerbation of asthma (history of asthma not previously documented).
- Secondary Considerations: Possible underlying respiratory infection or allergic reaction contributing to symptoms.
Plan
- Medications:
- Prescribe Albuterol inhaler for acute symptoms.
- Consider starting a low-dose inhaled corticosteroid for asthma management.
- Lifestyle Modifications:
- Advise on weight management and dietary adjustments to improve diabetes control.
- Encourage regular physical activity as tolerated.
- Follow-Up:
- Schedule a follow-up appointment in two weeks to re-evaluate symptoms and response to treatment.
- Recommend a pulmonary function test (PFT) if symptoms persist.
- Patient Education:
- Educate the patient about asthma management, recognizing triggers, and when to seek emergency care.
Part 5: Reflections
- What steps did you use to analyze the patient data?
- Why it’s important to notice patterns or discrepancies?
- How they would use this skill in a real healthcare setting.
Share your reflections to the class.

